INTRODUCTION
Transformations that have been occurring in society have had significant impacts on schools and on the teaching-learning relationship. These transformations necessitate changes to enable rapid and effective responses to the demands of students, who in turn live in an increasingly crowded environment with an increasingly unpredictable business world and rapid technological evolution. To keep up with these transformations in the student profile, and especially to keep the students engaged during the class period, in 2016 the “Universidade Anhembi Morumbi (UAM)”, located in São Paulo, Brazil, and a member of Laureate International Universities, implemented an extensive review of its Medical Curriculum and created a module called Genetic Basis of Medicine. This course is taken by the second semester and covers basic concepts and mechanisms from genetics/molecular biology, laboratory methods for genetic analyses, and the most relevant genetic diseases. The module structure is based on several different pedagogical approaches, including lectures, practical and experimental sessions in the wet laboratory, and active-learning methodologies. Active-learning methodologies are a growing trend in undergraduate teaching and are intended to promote higher cognitive level knowledge and development of soft skills (1,2). Team-Based Learning (TBL) is one of these methods and, since it was described by Larry Michaelsen, TBL has been successfully implemented in many Health Schools’ curricula (3,4) including Dentistry, Pharmacy, Veterinary Science/Medicine, Nursing, and Medicine (5–8). Moreover, in Medicine, many clinical and preclinical disciplines have been explored using TBL (9), including anatomy, ophthalmology, neurology, pathology, ethics, and pharmacology (10–14).
Team-Based Learning is learner-centered but instructor-led, uses a very structured individual and group accountability process, and requires small groups to work together to solve problems (15). It has been described as a cooperative learning method that can be applied to large groups where students work together in teams of five to seven people (16). The activity progresses from individual work, through group discussion and, finally, to discussion among the whole class in a continuous effort to gradually raise the cognitive level and increase the depth of the discussion (17). A TBL session is made up of three phases. It begins with the preparatory phase, in which students are given material to study before they come to class. The students then take readiness assurance tests (RAT), both an individual (iRAT) and a team (tRAT) conceptual test designed to assess their understanding of the pre-class material. Finally, in the team application phase (tAPP), they apply what they have learned by solving meaningful case-based exercises. During the session, the facilitator gives feedback, initiates discussions about the subject and encourages students to work in teams to apply the knowledge formally assessed during the iRAT and tRAT (18).
Team-Based Learning sessions are being used in other universities’ medical schools’ preclinical curricula (19,20), including in Medical Genetics teaching (21), but there are few studies. This study describes a Medical Genetics course organized into 5 blocks of subject matter on a total of 25 genetic diseases in which we used TBL sessions with first-year medical students. It reports on the students’ perceptions about and satisfaction with these sessions over two different years, showing that most of them approved of the format and believed that TBL was helpful to their learning experience.
METHODS
With institutional review board approval, first-year medical students (n= 290) studying at UAM in 2016/2017 were selected to participate in this study. Based on the NBEM (National Board of Medical Examiners) medical genetics topics and the university curriculum, twenty-five genetic diseases were grouped into five TBL sessions, according to their genetic causes (Table 1). The learning objectives for this subject were carefully adhered to, and materials were prepared in accordance with them. The TBL sessions accounted for around 1/6 of total course hours, and the remaining hours were dedicated to lectures, active-learning methods (other than TBL), experimental classes in the wet laboratory, and assessments.
TABLE 1 Distribution of subjects studied in each TBL session
| TBL #1 | TBL #2 | TBL #3 | TBL #4 | TBL #5 |
|---|---|---|---|---|
| DOMINANT AUTOSOMAL DISEASES | RECESSIVE AUTOSOMAL DISEASES | X-RELATED INHERITANCE DISEASES | STRUCTURAL CHROMOSOMAL ABNORMALITIES | NUMERICAL CHROMOSOMAL ABNORMALITIES |
| MARFAN SYNDROME #154700 | CYSTIC FIBROSIS #219700 | MUSCULAR DYSTROPHY, DUCHENNE TYPE #310200 | CRI-DU-CHAT SYNDROME #123450 | EDWARDS SYNDROME* |
| HUNTINGTON DISEASE #143100 | GAUCHER DISEASE #230800 | FRAGILE X SYNDROME #300624 | WOLF-HIRSCHHORN SYNDROME #194190 | PATAU SYNDROME* |
| NEUROFIBROMATOSIS #162200 | HEMOCHROMATOSIS #235200 | HEMOPHILIA A / B #306700/306900 | ANGELMAN SYNDROME #105830 | DOWN SYNDROME* |
| RETINOBLASTOMA #180200 | TAY-SACHS DISEASE #272800 | ORNITHINE TRANSCARBAMYLASE DEFICIENCY #311250 | PRADER-WILLI SYNDROME #176270 | TURNER SYNDROME* |
| ACHONDROPLASIA #100800 | PHENYLKETONURIA #261600 | GLUCOSE-6-PHOSPHATE DEHYDROGENASE DEFICIENCY #300908 | MILLER-DIEKER LISSENCEPHALY SYNDROME #247200 | KLINEFELTER SYNDROME* |
*information available for textual search at https://ghr.nlm.nih.gov/. All codes shown as # can be found at https://www.omim.org/.
For TBL sessions, the students were divided into groups of five to seven people on the first day, and these groups remained unchanged for the entire semester. Students were allocated to TBL teams at random, to reduce potential discrepancies in terms of students’ gender, regional status, and science background. Students were allowed one week to prepare for each session, by reading the book chapters recommended previously, and kindly reminded through institutional system Blackboard. The books were available at University’s Library (OTTO, P.A. et. al. Genética Médica. São Paulo:Roca, 2013 and NUSSBAUM, R.L. et. al. Thompson & Thompson – Genética Médica. São Paulo: Elsevier, 2016), which focused on the genetic mechanisms of disease, signs and symptoms, treatment and inheritance patterns. During each TBL session, students were asked to answer a set of 10 questions to test their understanding of the subject. A single faculty member facilitated sessions with groups of 55-70 students. Sessions started with an iRAT and then students were immediately divided into groups and took the tRAT. Both tests comprised the same 10 questions and after the tRAT phase the facilitator provided feedback and led a discussion of misconceptions. The groups’ answers were readily assessed using a set of cards bearing letters, which the groups raised to indicate their answers to each question. In the team application phase (tAPP), students discussed 5 cases related to the lesson in small groups. They then debated their answers in the large group and were given feedback by facilitators (Figure 1). For each clinical case, students were required to solve application questions related to disease diagnosis, molecular basis, and outcomes. This phase was developed following the 4S’s principles for tAPP (15). The complete TBL session lasted around 150 minutes, with an extra 20 minutes in the beginning (for divide students, distribute score sheets and prepare equipment such as computer and data show); and 30 minutes at the end to solve questions, orient students to the next session and fill class diary. The time spent was similar to other methodologies.
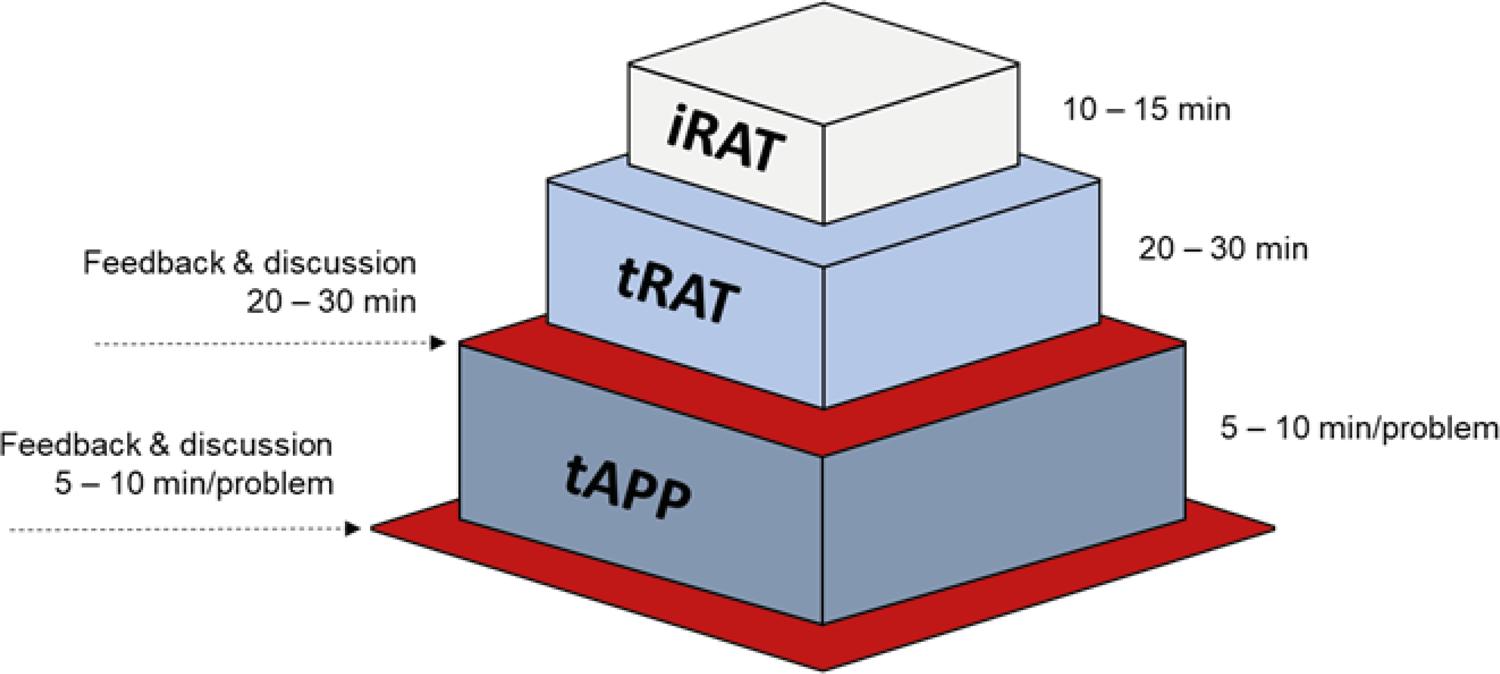
FIGURE 1 TBL session structure. For iRAT we used 10 multiple choice questions. The same questions were used for tRAT. For tAPP we used five clinical cases, related to each genetic disease
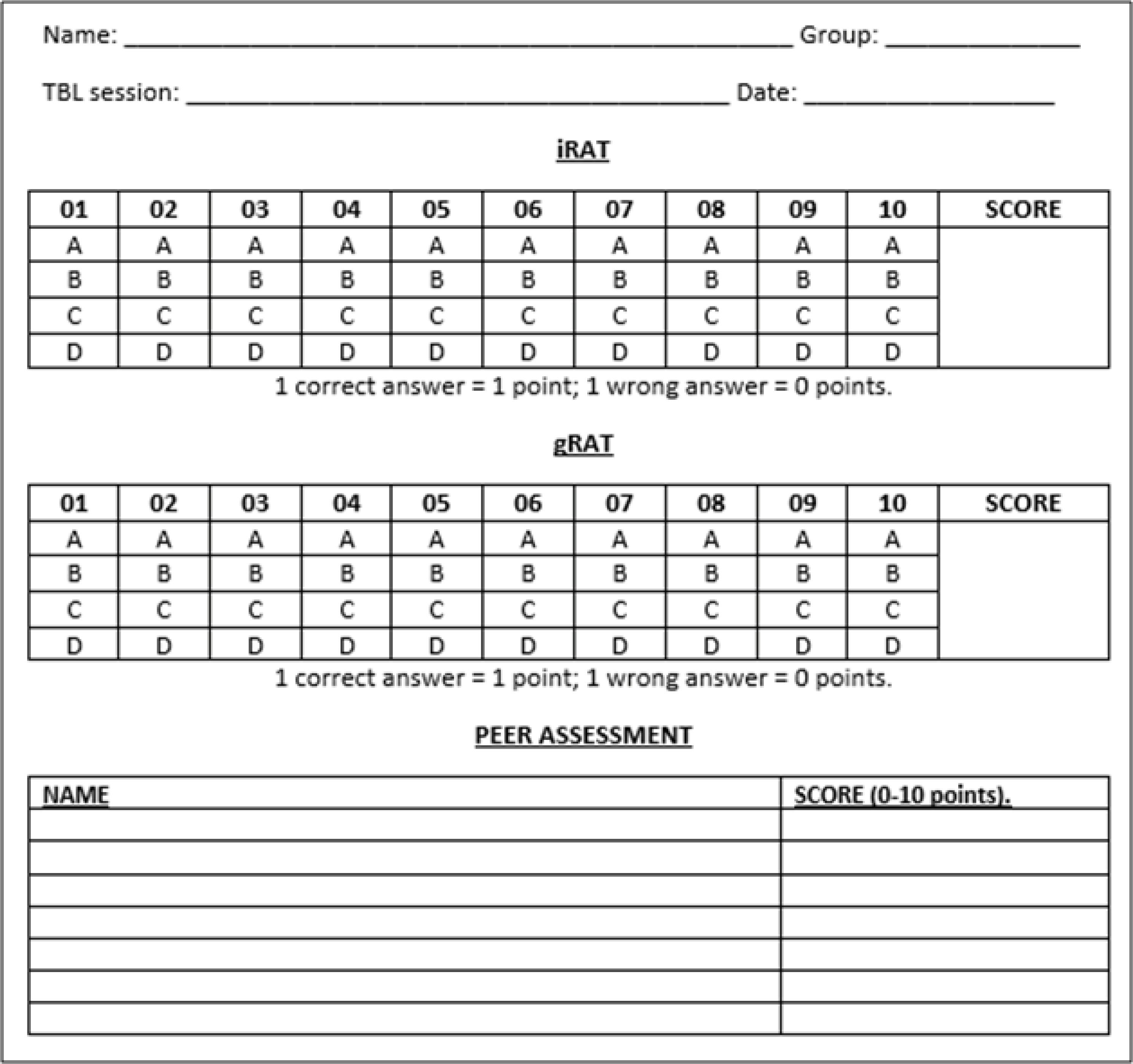
Students were scored for iRAT, tRAT and by peer assessment at the end of the session, as follows: iRAT (60% of total score), tRAT (30% of total score), and peer assessment (10% of total score). For the peer assessments, each student was requested to award a score from 0 to 5 points to each of the other students in their group for 2 criteria and to sum the scores for each student (a maximum total of 10 points), as follows: I) the student demonstrates theoretical mastery of the subject; and II) the student contributed to the group achieving a good outcome. The form shown in Figure 2 was used for TBL assessments.
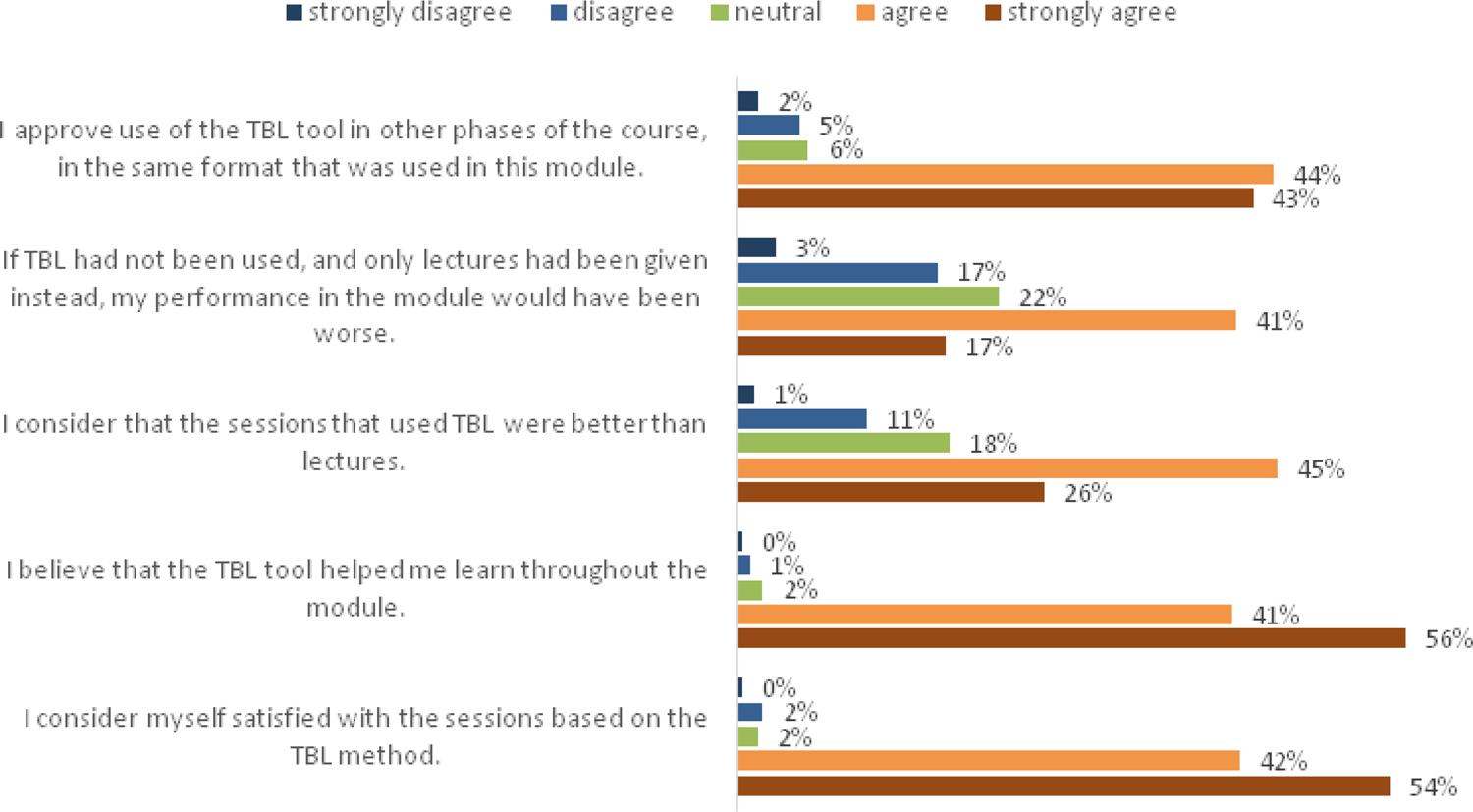
At the end of the semester, the students were asked to answer a questionnaire comprising five questions. For each item, they could choose strongly agree, agree, neutral, disagree, or strongly disagree with the following statements: I) I consider myself satisfied with the sessions based on the TBL method; II) I believe that the TBL tool helped me learn throughout the module; III) I consider that the sessions that used TBL were better than lectures; IV) If TBL had not been used, and only lectures had been given instead, my performance in the module would have been worse; and V) I approve use of the TBL tool in other phases of the course, in the same format that was used in this module. They were also requested to complete a consent form granting permission for their data to be used for research and publication. We evaluated two different and independent groups of students who had concluded the course by 2016 and 2017 respectively, totaling 290 students overall. Data were transferred to an Excel spreadsheet and used to generate charts. The research project was approved by the ethics committee at Universidade Anhembi Morumbi under report number 2.868.342.
RESULTS
A total of 290 participants completed a questionnaire on their TBL experience. Student responses to closed items are shown in Figure 3. Overwhelmingly, the students agreed that TBL sessions helped them to learn throughout the semester, with 96% strongly agreeing or agreeing that “I consider myself satisfied with the sessions based on the TBL method”. Importantly, students also believed that the TBL tool helped them learn throughout the module, since 97% strongly agreed or agreed with that statement. Notably, 71% of students strongly agreed or agreed with the statement “I consider that the sessions that used TBL were better than lectures”. Additionally, 58% agree or strongly agree with the statement “If TBL had not been used, and only lectures had been given instead, my performance in the module would have been worse”. Finally, 87% strongly agreed or agreed with the sentence “I approve use of the TBL tool in other phases of the course, in the same format that was used in this module.”. Moreover, Table 2 shows that the students who strongly agreed with each question had high rates of positive answers in all of the other questions, showing the students’ agreement with the questionnaire.
TABLE 2 Pattern of responses of students who strongly agree with each question
| % of students, among those who strongly agree with each question who also gave positive answers to other questions. | ||||||
|---|---|---|---|---|---|---|
|
| ||||||
| Q1 | Q2 | Q3 | Q4 | Q5 | ||
| No. Of students who strongly agree in each question | Q1 (N=157) | – | 99.3% | 75.7% | 73.2% | 94.9% |
| Q2 (N=161) | 100.0% | – | 81.3% | 74.5% | 95.0% | |
| Q3 (N=74) | 100.0% | 100.0% | – | 79.7% | 95.9% | |
| Q4 (N=50) | 100.0% | 100.0% | 92.0% | – | 96.0% | |
| Q5 (N=124) | 99.1% | 99.1% | 82.2% | 73.3% | – | |
Furthermore, students made open comments when completing the questionnaire, some examples of which are show below. The students listed the following aspects of their TBL experience as positive: smaller group size (5 – 7); immediate feedback from the facilitator; efficient use of time, greater likelihood that they would arrive at the class prepared; and improved quality of team and class discussion because students were better prepared in advance.
“…the lessons were very well delivered and the results of TBL were very satisfactory...”
“...I hope to continue with this model of classes, since the semester was very good...”
“...I consider the TBL method, with discussion of clinical cases in groups, very good....”
“...by encouraging autonomous research, the TBL method amplifies curiosity about a certain subject, so that students do not restrict themselves to the questions asked...”
“...the way it was used here, the TBL ensures that students are always up to date with the study schedule and helps them to study the subject in greater depth...”
DISCUSSION
There are few published results on genetics learning and TBL in the literature. Just one article describes a single session of TBL in an entire Medical undergraduate course, and the results showed that students’ performance in a group readiness test was better than in individual readiness tests. The effectiveness of TBL was also revealed in the examination, in which the marks obtained improved (21). Another study described three workshops for resident students in two different Pathology National Meetings addressing Genomic Pathology topics with relation to Breast Cancer and the results showed that TBL is a feasible and effective strategy for teaching genomic medicine that is acceptable to pathology residents at national meetings (22). In contrast with these one-off interventions, we describe two years’ continuous experience involving 25 Genetic Diseases, organized in 5 TBL modules, addressing Basic and Medical Genetics topics over an entire semester. In our study, the students’ perception of TBL sessions were positive and they felt that TBL helped them to learn about medical genetics.
Students’ perceptions, together with students’ attitude and learning outcomes are the aspects most studied in researches on TBL (24). We found that TBL provided a good learning experience for our students, almost in totality. While many publications corroborate our data (23,25–29), a small, but representative, number report divergent results, describing negative experiences with TBL (30,31). Here, 96% of students got satisfied with TBL sessions, 97% agreed that TBL helped them to learn and 87% approved the use of TBL in other moments in the future. However, around 30% do not agreed that TBL sessions were better than lecture and 42% do not agreed that they performance were improved by TBL. This fact can reflect student’s resistance to active methodologies. The Genetic’s Course were offered in second semester of Medical curriculum, and offering TBL early in the curriculum prior to traditional lecture-based formats is better received by students (23).
The authors of a recent systematic review (24) evaluated relevant published literature on TBL. Their results showed that 72% of the articles included assessed learning outcomes and most of the articles involved undergraduate medical students. Of these, 61% (52/85) concluded that TBL was an effective instructional technique. Although we did not address learning outcomes, our students performed well in TBL assessments and obtained high pass rates on our course, which suggests TBL is effective. Previous studies have found that tRAT scores were higher than iRAT scores. The review authors pointed out that this finding is to be expected since in the tRAT portion of TBL students are able to discuss the answers and gain from each other’s knowledge (24). It is important to emphasize that just one study was from Brazil and the field of genetics doesn’t figure among TBL published topics, showing that studies related to the field of genetics are important to improve medical education in this area.
We implemented a hybrid module of Medical and Basic Genetics built around TBL and LBL (Lecture-Based Learning), since each TBL was preceded by a Lecture addressing topics related to diseases that students would cover in the next session. Yang and colleagues (32) demonstrated better learning outcomes using this model than with TBL or LBL alone. Another feature of our model was that we used a full-credit assessment method for iRAT and tRAT. In general, students scored well on both iRAT and tRAT TBL sessions, but Farland and colleagues (33) demonstrated that when using an answer-until-correct assessment method rather than traditional full-credit methods, the student scored significantly lower in iRATs and achieved similar scores on tRATs. Meanwhile, students who used the answer-until-correct method had higher quality team interaction ratings and better scores in final team examinations. In our experience, the full-credit assessment was easier and less laborious for the professor to account for students (given the group size and the limited number of professors).
In our TBL sessions, students took iRAT, tRAT, and tAPP in the classroom. However, while this is the most common approach and for tRAT and tAPP, the need for group interaction undoubtedly suggests that the activity should take place in the classroom, this is not entirely true for iRAT. According to Carbrey and colleagues (34), in a physiology course, students’ performance after at-home iRAT was equivalent to performance after traditional in-class iRAT. We chose to apply iRAT in class because this was the first time that this method was used systematically, and we wished to avoid bias and/or misconceptions about the methodology and engage students in an immersive full-time in-class experience close to the facilitator.
During TBL session facilitation, we paid close attention to the feedback points, after tRAT and between application questions. Another study reinforces the impact of feedback modality, written and/or verbal. The data suggest that written and verbal explanations may help students more than written feedback alone. The same study also suggests that receiving written comments alone may have confused participants (35). We only gave verbal feedback to students, based on a very short lecture on those questions that groups had answered incorrectly. We believe that this approach does not eliminate the need to provide written feedback, but the lack was mitigated by the fact that students could take notes during the teacher’s explanation and ask questions to resolve specific doubts. It has been observed that when learners are given written as well as verbal feedback on their performance in class, facilitator feedback in TBL makes the greatest difference to their pre-test to post-test score improvement, when compared to either just written feedback or no feedback at all (35).
Implementing the TBL method in the curriculum can be a hard task for faculty, but it is rewarding and beneficial to student learning and skills (36,37). Over recent years, the number of studies on active learning methods (especially TBL) for health professions education has grown dramatically (24). This is indicative of the growing interest in moving health profession education away from strict memorization toward meaningful learning experiences and critical thinking. Since curricula have been reviewed and active methodologies have been implemented in many different courses, we can assume that these desires can be achieved.
CONCLUSION
Based on the perceptions of the medical students involved in the study, implementation of TBL in our institution has resulted in positive outcomes. In the future, it would be interesting to evaluate the effect of TBL on student performance. This study reinforces and improves the existing evidence on implementation of TBL in Medical Schools and illustrates that the TBL experience in a hybrid curriculum format was well received by students and positively impacted their perceptions of learning.