Serviços Personalizados
Journal
Artigo
Compartilhar
Revista Brasileira de Educação Médica
versão impressa ISSN 0100-5502versão On-line ISSN 1981-5271
Rev. Bras. Educ. Med. vol.47 no.4 Rio de Janeiro 2023 Epub 20-Nov-2023
https://doi.org/10.1590/1981-5271v47.4-2022-0196
ORIGINAL ARTICLE
In situ simulation and its different applications in healthcare: an integrative review
1 Universidade de São Paulo, São Paulo, São Paulo, Brazil.
2 Universidade Federal do Maranhão, São Luís, Maranhão, Brazil.
3 Universidade do Oeste Paulista, Presidente Prudente, São Paulo, Brazil.
Introduction:
The in situ simulation (ISS) consists of a training technique that takes place in the real workplace as a relevant method to promote environmental fidelity in the simulated scenario.
Objective:
To verify the use of the ISS in the world, to understand its applicability in healthcare.
Method:
This is an integrative review, which used the following guiding question: How has in situ simulation been used by health professionals? Searches were carried out in the PubMed, SciELO, LILACS and Web of Science databases, with different combinations of the following descriptors: in situ simulation, health and medicine (in Portuguese, English and Spanish) and the Boolean operators AND and OR using a temporal filter from 2012 to 2021. A total of 358 articles were found and the inclusion and exclusion criteria were applied, following the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA), and also with an independent peer review, using Rayyan, leaving 190 articles for this review.
Results:
The results showed that the United States has the absolute majority of productions (97/51%), followed by Canada, but with a large numerical difference (18/9.5%). Most of the works are written in English (184/96.8%), are quasi-experimental studies (97/51%), and have multidisciplinary teams as the target audience (155/81.6%). The articles have 11,315 participants and 2,268 simulation interventions. The main ISS scenarios were the urgent and emergency sectors (114/60%), followed by the ICU (17/9%), delivery room (16/8.42%) and surgical center (13/6.84%). The most frequently studied topics were CPR (27/14.21%), COVID-19 (21/11%), childbirth complications (13/6.8%) and trauma (11/5.8%).
Discussion:
The pointed-out advantages include the opportunity for professional updating with the acquisition of knowledge, skills and competencies, in an environment close to the real thing and at low cost, as it does not depend on expensive simulation centers.
Conclusion:
In situ simulation has been used by health professionals worldwide, as a health education strategy, with good results for learning and training at different moments of professional training, with improved care and low cost. There is still much to expand in relation to the use of ISS, especially in Brazil, in the publication of studies and experience reports on this approach.
Keywords: Simulation Training; High Fidelity Simulation Training; Health Human Resource Training; Work Engagement
Introdução:
A simulação in situ (SIS) consiste em técnica de capacitação que ocorre no local real de trabalho como um método relevante para promover a fidelidade ambiental no cenário simulado.
Objetivo:
Este estudo teve como objetivo verificar o uso da SIS no mundo para compreender sua aplicabilidade na área de saúde.
Método:
Trata-se de uma revisão integrativa que adotou a seguinte questão norteadora: “Como tem sido utilizada a simulação in situ por profissionais da área da saúde?”. Foram realizadas buscas nas bases PubMed, SciELO, LILACS e Web of Science, com as diferentes combinações dos descritores “simulação in situ”, “saúde” e “medicina” (em português, inglês e espanhol) e os operadores booleanos AND e OR, com utilização de filtro temporal de 2012 a 2021. Encontraram-se 358 artigos, nos quais se aplicaram os critérios de inclusão e exclusão, seguindo as recomendações do Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA). Após revisão independente realizada por pares, com o uso do Rayyan, restaram 190 para esta revisão.
Resultado:
Os resultados mostraram que os Estados Unidos detêm a maioria absoluta das produções (97/51%), seguidos do Canadá, porém com grande diferença numérica (18/9,5%). A maior parte dos trabalhos está escrita em inglês (184/96,8%), é quase experimental (97/51%) e tem equipes multiprofissionais como público-alvo (155/81,6%). Os artigos têm 11.315 participantes e 2.268 intervenções de simulação. Os principais cenários de SIS foram os setores de urgência e emergência (114/60%), seguidos de UTI (17/9%), sala de parto (16/8,42%) e centro cirúrgico (13/6,84%). Os temas mais estudados foram RCP (27/14,21%), Covid-19 (21/11%), complicações do parto (13/6,8%) e trauma (11/5,8%). As vantagens apontadas incluem: atualização profissional e aquisição de habilidades e competências em ambiente próximo do real e de baixo custo por não depender de dispendiosos centros de simulação.
Conclusão:
Em todo o mundo, a SIS tem sido utilizada por profissionais da saúde como estratégia de educação na área de saúde, com bons resultados para aprendizagem e capacitações de diferentes momentos da formação profissional e com melhora da assistência. Ainda há muito o que expandir em relação ao uso da SIS, sobretudo no Brasil, na publicação de estudos sobre essa abordagem.
Palavras-chave: Treinamento por Simulação; Treinamento com Simulação de Alta Fidelidade; Capacitação de Recursos Humanos em Saúde; Engajamento no Trabalho
INTRODUCTION
Simulation is an increasingly recognized tool for teaching, training and assessing healthcare professionals. Having been used for many years to improve clinical care and teamwork, simulation can be carried out in different environments: off-site (simulation centers or other locations far from clinical units) or in situ (real clinical environment)1.
In situ simulation (ISS) consists in a training technique that takes place in the real workplace, along the same lines as traditional clinical simulation, including the briefing steps (contextualization and detailing of the simulated scenario before application), development of the simulated scenario and debriefing (dialogues after the practice aiming at promoting reflection). It is a very promising method to promote the environmental fidelity of those involved in the simulated scenario2.
When carried out at the professional place of work, the ISS allows evaluating the practical and critical thinking skills of a healthcare team in their work environment, encouraging the improvement of clinical practices3. Moreover, it allows the institution to address a series of aspects related to the healthcare processes, organizational efficiency and operational safety, including the identification of latent hazards, knowledge gaps, unmet equipment needs, environmental issues and space constraints, as well as a multitude of issues linked to human resources4.
There is evidence of benefits, including those related to the perceived self-efficacy, that is, the perception of technical advances related to training. National studies have shown that professionals perceived the in situ simulation strategy as valid for professional updating and practical learning in a safe environment5)-(8. At the international level, it can be observed that simulation is widely practiced at different levels of care9),(10, also as a quick and efficient tool to implement protocols in cases of outbreaks11)-(16 and can also be an acceptable approach for training the interprofessional team in primary care17.
Despite these findings, simulation continues to be carried out preferably in simulation centers. This practice requires the presence of these spaces, technological resources and the availability of trained personnel to conduct them, which, in the vast majority of cases, do not exist in health services. This prevents the development of simulation activities by professionals who work in patient care9. In places that adopted ISS in their routine, the fidelity of the scenario showed a clear advantage, with a great impact on the transfer of knowledge to participants in simulated practices18.
It is worth highlighting that the simulation carried out in simulation centers is usually related to a curriculum or the development of technical and non-technical skills in undergraduate or continuing education spaces. In this context, the inclusion of training for care teams with a focus on the health network, rather than individuals or failures, emphasizes teamwork and the development of instruction, investigation, workload distribution, surveillance and conflict resolution skills19.
The use of clinical simulation is recent in universities, medical schools and other areas of health in Brazil. The National Curricular Guidelines for Medical Courses of 2001 and 2014 were attempts to change this scenario, promoting greater integration between teaching-service-community and providing prior skills training, through simulation, anticipating contact with real patients20.
Training non-technical skills is much more than just a simulation activity. This training is loaded with such a plurality of skill areas, topics, multiple configurations for training and assessment procedures that it becomes a possible process to define common values and fundamental standards necessary for professional activity21. The ISS aims to enable teams to review and improve their skills in the real clinical environment22.
There are few researchers dedicated to the topic in Brazil5)-(8, and these are usually linked to academia and not to health care services, which may lead to the underutilization of this tool for developing better assistance by multidisciplinary health teams23.
Therefore, as ISS is an emerging and promising learning strategy in education for health professionals, it is relevant to identify how it has been used worldwide. This study aims to understand its applicability in different environments, topics and health areas worldwide, identifying the situation in Brazil in this context.
METHOD
The integrative review was the method chosen due to its potential to capture the complexity of broad and varied perspectives of a studied phenomenon. The study followed the following steps: problem identification, literature search, data evaluation, data analysis and presentation24. It was also based on the recommendations of the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA)25.
For data collection, the PICO (Patient, Intervention, Comparison and Outcomes) strategy was used, with the following guiding question: “How has in situ simulation been used by health professionals?”. Searches were carried out in the following databases: PubMed, Scientific Electronic Library Online (SciELO) and Latin American and Caribbean Literature in Health Sciences (LILACS) and Web of Science.
Once the terms and their combinations were adopted (Chart 1), the searches were limited to studies published from 2012 to 2021, considering that relatively recent articles can more accurately translate the context of in situ simulation used by health professionals worldwide. The last search in the consulted databases was carried out on March 11, 2022.
Chart 1 Literature search strategy based on the chosen databases.
| Databases | Search terms |
|---|---|
| PubMed | “in situ simulation” |
| LILACS | “in situ simulation” OR “simulação in situ” OR “simulación in situ” |
| SciIELO | “in situ simulation” OR “simulação in situ” OR “simulación in situ” |
| Web Of Science | “in situ simulation” AND (Health OR Medical) |
Source: prepared by the authors.
In the LILACS and SciELO databases, the strategy of expanding the search was adopted by translating the term “in situ simulation” into Portuguese and Spanish, as they are bases that accept multiple languages in their indexing. On Pubmed, the term ‘in situ simulation’ was maintained in English as, on this platform, the variation in translation of the term did not change the search result. In the Web of Science database, the search for results within health topics was restricted, as it is a storage site with the possibility of results in the most diverse areas of knowledge.
Considering that the study analyzed studies on simulation used by healthcare professionals within their work environment, the ones that dealt with simulations carried out in a simulation center and other environments (off-site) and in situ simulations carried out by other areas of knowledge were excluded. Moreover, the following were also excluded: (a) articles in duplicate; (b) studies considered gray literature (editorials, theses and annals); (c) publications whose participants were not health professionals; (d) studies that deviated from the main topic, despite containing the topic of in situ simulation in the body of the text; (for example: simulation of cell proliferation in situ); (e) literature reviews.
When divided by databases, the platforms showed the following results, respectively: LILACS 19, SciELO 8, Web of Science 270, Pubmed 61, totaling 358 articles.
These 358 articles were exported to the Rayyan systematic review program to facilitate peer review26.
The program indicated 34 articles in duplicate, seven of which were automatically excluded, as they were considered exact duplications, and 27 were indicated for analysis by the reviewers, who considered 26 articles as duplications, totaling the exclusion of 33 articles according to this criterion.
The analysis of the remaining 325 articles occurred by reading the titles and abstracts through independent reading by two authors, and as there was no disagreement between them, 127 articles were excluded and 198 were selected for reading in full, with a further eight articles being excluded, thus leaving 190 articles to comprise the sample. The selection process for articles included in this review is shown in the PRISMA25 flowchart below (Figure 1).
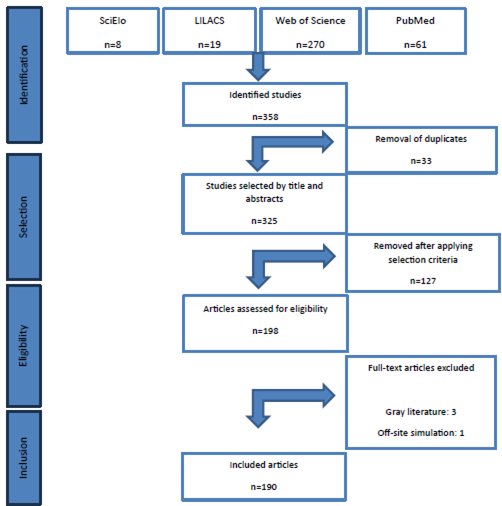
Source: Prepared by the authors based on the PRISMA25 recommendation.
Figure 1 Flowchart of steps used for sample selection.
The authors independently read the articles included in the sample to extract data using a specific form created to gather the following information: Author; Country of study; Continent; Language; Journal; Years of publication compiled into blocks; Study design; Level of Evidence (level I - meta-analyses of controlled and randomized clinical studies; level II - experimental design study; level III - quasi-experimental studies; level IV - qualitative non-experimental studies or descriptive studies; level V - case reports or experience reports; and level VI - expert opinions or based on regulatory or legal standards)27; Goal; Target Audience; Objective of the intervention; Methodology used; Number of participants; Number of simulation sessions; Thematic area (surgery, internal medicine, pediatrics, collective health or gynecology and obstetrics); Place of performance; Covered topic; Results and Conclusions.
To organize the information, studies with a quantitative, qualitative and mixed methods approach were differentiated. Subsequently, a narrative synthesis of the data was carried out using thematic analysis28.
RESULTS
Table 1 shows the characterization of the selected studies, according to continent, language, year of publication, type of study and level of evidence, demonstrated by numbers and corresponding percentages.
Table 1 Characterization of the selected studies, according to continent, language, year of publication, type of study and level of evidence.
| Characteristics | Frequency | % | Cumulative |
|---|---|---|---|
| Continent | |||
| North America | 115 | 60.53 | 115 |
| South America | 8 | 4.21 | 123 |
| Africa | 3 | 1.58 | 126 |
| Europe | 43 | 22.63 | 169 |
| Asia | 16 | 8.42 | 185 |
| Oceania | 5 | 2.63 | 190 |
| Antarctica | 0 | 0 | 190 |
| Total | 190 | 100% | 190 |
| Language | |||
| English | 184 | 96.84 | 184 |
| Spanish | 2 | 1.05 | 186 |
| Portuguese | 4 | 2.11 | 190 |
| Others | 0 | 0 | 190 |
| Total | 190 | 100% | 190 |
| Year of publication | |||
| 2012 - 2013 | 7 | 3.68 | 7 |
| 2014 - 2015 | 24 | 12.63 | 31 |
| 2016 - 2017 | 25 | 13.16 | 56 |
| 2018 - 2019 | 53 | 27.90 | 109 |
| 2020 - 2021 | 81 | 42.63 | 190 |
| Total | 190 | 100% | 190 |
| Type of study and level of evidence | |||
| Experimental study - II | 8 | 4.21 | 8 |
| Quasi-experimental study - III | 97 | 51.05 | 105 |
| Descriptive study - IV | 63 | 33.16 | 168 |
| Qualitative study - IV | 11 | 5.79 | 179 |
| Mixed study - IV | 7 | 3.68 | 186 |
| Experience report - V | 4 | 2.11 | 190 |
| Total | 190 | 100% | 190 |
Source: prepared by the authors.
The analysis of the articles showed that the United States has the absolute majority, with 97 articles (51%), followed by Canada with 18 articles, showing a large numerical difference (9.5%). Only seven studies (3.7%) were conducted in Brazil. Thus, the majority of the 184 studies are written in English (96.8%), with four in Portuguese (2.1%) and two in Spanish (1%).
An increase in publications was observed in the last four years (70.53%), showing that ISS has been more applied and studied.
When the studies are divided according to type, the majority of 97 (50.05%) were quasi-experimental, with level of evidence III, followed by 63 descriptive studies (33%), and 11 qualitative ones (5.8%), both with level of evidence IV (38.8%).
Regarding the target audience, studies involving multidisciplinary teams predominated, with 155 publications (81.6%), followed by nursing, with only 14 studies (7.4%).
Table 2 shows the characterization of the studies based on thematic areas, according to the target audience, covered topic and scenario/sector.
Table 2 Characterization of studies based on thematic areas, according to target audience, covered topic and scenario/sector.
| Internal medicine n:71 | Pediatrics n:59 | Surgery n: 20 | Others/ Multiplea n:18 | Obstetrics n:16 | Anesthesiology n:1 | Mental health n:1 | Collective health / Family medicine n:4 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Público Alvo | |||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | TOTAL | |
| Multiprofessional team | 56 | 78. 9 | 49 | 83.0 | 17 | 85.0 | 18 | 100.0 | 11 | 68.75 | 0 | 0 | 1 | 100.0 | 3 | 75.0 | 155 |
| Nurses | 8 | 11.3 | 2 | 3.4 | 1 | 5.0 | 0 | 0 | 2 | 12.5 | 0 | 0 | 0 | 0 | 1 | 25.0 | 14 |
| Physicians | 2 | 2.8 | 2 | 3.4 | 1 | 5.0 | 0 | 0 | 1 | 6.25 | 1 | 100.0 | 0 | 0 | 0 | 0 | 7 |
| Medical Residents | 2 | 2.8 | 1 | 1.7 | 1 | 5.0 | 0 | 0 | 1 | 6.25 | 0 | 0 | 0 | 0 | 0 | 0 | 5 |
| Undergraduate students | 2 | 2.8 | 4 | 6.8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| Others | 1 | 1.4 | 1 | 1.7 | 0 | 0 | 0 | 0 | 1 | 6.25 | 0 | 0 | 0 | 0 | 0 | 0 | 3 |
| Total | 71 | 100% | 59 | 100% | 20 | 100% | 18 | 100% | 16 | 100% | 1 | 100% | 1 | 100% | 4 | 100% | 190 |
| Covered topic | |||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | TOTAL | |
| CPR | 13 | 18.3 | 14 | 23.7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 27 |
| COVID 19 | 17 | 23.9 | 0 | 0 | 1 | 5.0 | 2 | 11.1 | 0 | 0 | 1 | 100.0 | 0 | 0 | 0 | 0 | 21 |
| Trauma | 2 | 2.8 | 3 | 5.1 | 6 | 3.0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 11 |
| Sepsis | 3 | 4.3 | 3 | 5.1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| Delivery complications | 0 | 0 | 1 | 1.7 | 0 | 0 | 1 | 5.5 | 11 | 68.75 | 0 | 0 | 0 | 0 | 0 | 0 | 13 |
| Patient safety | 1 | 1.4 | 0 | 0 | 2 | 5.0 | 3 | 16.7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 6 |
| Others | 35 | 49.3 | 38 | 64.4 | 11 | 55.0 | 12 | 66.7 | 5 | 31.25 | 0 | 0 | 1 | 100.0 | 4 | 100.0 | 106 |
| TOTAL | 71 | 100% | 59 | 100% | 20 | 100% | 18 | 100% | 16 | 100% | 1 | 100% | 1 | 100% | 4 | 100% | 190 |
| Sector | |||||||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | TOTAL | |
| Urgency / Emergency | 54 | 76.0 | 40 | 67.8 | 10 | 50.0 | 7 | 39.0 | 3 | 18.75 | 0 | 0 | 0 | 0 | 0 | 0 | 114 |
| Delivery room | 0 | 0 | 6 | 10.2 | 0 | 0 | 1 | 5.5 | 9 | 56.25 | 0 | 0 | 0 | 0 | 0 | 0 | 16 |
| ICU / CCU | 8 | 11.3 | 8 | 13.5 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 100.0 | 0 | 0 | 0 | 0 | 17 |
| Surgical center | 0 | 0 | 0 | 0 | 10 | 50.0 | 1 | 5.5 | 2 | 12.5 | 0 | 0 | 0 | 0 | 0 | 0 | 13 |
| Ambulatory | 2 | 2.8 | 1 | 1.7 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 75.0 | 6 |
| Ward | 3 | 4.3 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 6.25 | 0 | 0 | 1 | 100.0 | 0 | 0 | 5 |
| Others | 4 | 5.6 | 4 | 6.8 | 0 | 0 | 9 | 50.0 | 1 | 6.25 | 0 | 0 | 0 | 0 | 1 | 25.0 | 19 |
| TOTAL | 71 | 100% | 59 | 100% | 20 | 100% | 18 | 100% | 16 | 100% | 1 | 100% | 1 | 100% | 4 | 100% | 190 |
aWithin this category, data relating to articles that had application to multiple teams and which articles were not clear regarding the relevance and quantification of participants in each area were included. Therefore, these are studies that talk about its systematic application in different areas in health services.
Abbreviations: CPR - Cardiopulmonary resuscitation; ICU/CCU - Intensive Care Unit/Critical Care Unit
Source: prepared by the authors.
In relation to the place where the simulations were carried out, there was a predominance in the urgency and emergency sector, with 114 studies (60%), with the majority of simulations carried out in Internal Medicine with 54 studies (47.4%) and Pediatrics with 40 studies (35%). Next, we have the ICUs with 17 studies (9%), of which eight are in Internal Medicine (47%) and eight in Pediatrics (47%). The Delivery room had 16 studies (8.42%), of which nine studies were in Obstetrics (56.25%) and 6 in Pediatrics (37.5%). The Surgical center had 13 studies (6.84%), of which ten (76.9%) were in Surgery.
When we analyze the areas individually, we see that ISS has been most applied in Internal Medicine, with 71 studies (37.3%), followed by Pediatrics with 59 (31%) and Surgery with 20 (10.5%).
The most frequently discussed topics in the ISS, according to the studies, were CPR with 27 publications (14.2%), followed by COVID-19 with 21 publications (11%), delivery complications with 13 publications (6.8%) and trauma with 11 (5.8%).
Table 3 shows the characterization of the studies based on the type of intervention and number of simulated activities.
Table 3 Characterization of studies based on the type of intervention and number of simulated activities.
| Type of intervention | Frequency | % |
|---|---|---|
| Class/Demonstration | 12 | 6.3 |
| Continuing Education | 81 | 42.6 |
| Evaluation | 10 | 5.3 |
| Permanent Education | 85 | 44.7 |
| No information | 2 | 1.1 |
| Total | 190 | 100% |
| Simulated activities | Frequency | % |
| From 1 to 10 | 113 | 59.5 |
| From 11 to 20 | 26 | 13.7 |
| From 21 to 30 | 8 | 4.2 |
| From 31 to 40 | 8 | 4.2 |
| From 41 to 100 | 8 | 4.2 |
| > 100 | 5 | 2.6 |
| No information | 22 | 11.6 |
| Total | 190 | 100% |
Source: prepared by the authors.
Regarding the type of intervention, 85 (44.7%) studies were on permanent education (defined as such or that had regular activities), followed by 81 (42.6%) with isolated training, which were classified as continuing education.
Chart 2 shows the evidence associated with studies of continuing education interventions and, in general, it can be observed they are related to patients, the professionals’ technical and non-technical skills, patient safety and the teaching/learning process, as highlighted in the chart below:
Chart 2 Evidence associated with the studies that showed results of continuing education interventions.
| Evidence associated with patients | Better outcome for general emergency patients31; |
| Better blood glucose control for pediatric patients; | |
| Reduction in weighted mortality adjusted to the risk of septic shock32; | |
| Increase in the number of patients referred to the allergy unit33; | |
| Better patient comfort in the emergency department34. | |
| Evidence associated with the professionals’ technical skills | Improvement in pediatric airway management35; |
| Improved accuracy in recognizing signs and symptoms of patients with clinical deterioration and provision of effective initial interventions36; | |
| Increased adherence by professionals to different care guidelines10),(37),(38; | |
| Improvement in teamwork performance of professionals in resuscitation39)-(42; | |
| Improvement in the correct management of anaphylaxis33; | |
| Improvement in trauma simulation assessment scores43; | |
| Improving teamwork in intubation44; | |
| Improvement in the performance of pediatric trauma care45; | |
| Improvement in the timely use of resources when responding to crises13),(46; | |
| Improvement in levels of knowledge in ECMO47; | |
| Improved accuracy in recognizing signs and symptoms of patients with clinical deterioration and provision of effective initial interventions36; | |
| Evidence associated with the professionals’ non-technical skills | They contributed to a significant improvement in professionals’ confidence in relation to the procedures48)-(50; |
| Improved communication13),(46),(51),(52; | |
| Improved teamwork4),(22),(32),(39),(53)-(56; | |
| Improvement in leadership capacity57)-(59; | |
| Improvement in interprofessional collaboration60; | |
| Improves the identification of professionals’ roles49; | |
| Improving team familiarity with devices, equipment and environment61; | |
| Improvement in the professionals’ emotional response62; | |
| Improvement in the professionals’ comfort and satisfaction50),(63. | |
| Evidence associated with patient safety | Improvement in the identification of latent safety threats in the clinical care environment13),(46),(49),(64-(70; |
| Promotes a culture of patient safety22),(42),(71)-(75; | |
| It makes it possible to mitigate risks to patient safety2),(4),(64),(67),(76)-(79; | |
| Identify areas that require additional education to improve patient safety72),(80; | |
| Provides an environment to safely train interventions72),(81),(82. | |
| Evidence associated with the teaching-learning process. | Adequate use of educational resources83; |
| Better learning results61),(83-(85; | |
| Enables interprofessional education57; | |
| Allows adults to learn in a safe environment36; | |
| Reliable to evaluate the professionals’ clinical performance66),(86; | |
| Allows simulation training with few resources77),(72),(87),(88. |
Source: prepared by the authors.
It was possible to identify some advantages in the results related to in situ simulation as an opportunity to update and acquire knowledge, professional skills and competencies5. Other results include the improvement in teamwork and individual learning, and the ability to offer greater realism and transferability, at low cost61),(89),(90.
Furthermore, it allows improved performance in real clinical scenarios, helping to reveal important latent risks and the implementation of corrective measures77),(91),(92.
Considering the data extracted from the articles, a total that exceeds 2,268 simulation interventions and 11,315 participants stands out, since it was not possible to extract this information from 29 articles, as shown in Chart 3.
Chart 3 Characterization of the selected studies, according to the number of participants and number of simulated activities per thematic area.
| Thematic Area | Total Participants | Total Simulated Activities |
|---|---|---|
| Internal medicine | 3,851 | 988 |
| Pediatrics | 3,406 | 494 |
| Surgery | 1,293 | 516 |
| Obstetrics | 133 | 63 |
| Anesthesia | 12 | 36 |
| Mental Health | 53 | 8 |
| Collective health/Family medicine | 130 | 55 |
| Interprofessional/Others | 2,437 | 108 |
| Total | 11,315 | 2268 |
Source: prepared by the authors.
DISCUSSION
The use of ISS allowed the approach of several useful topics in the most different areas of knowledge, disciplines and cultures, being reproduced in different places worldwide, considering the fact that it respects and adapts to the characteristics of local services, without requiring large extra investments for its performance.
Moreover, it demonstrated several advantages related to its use, reinforcing literature findings and strengthening evidence that its use brings several benefits to care, professionals and patients, as demonstrated in other studies that used the ISS and stated significant gains in confidence, both for experienced professionals and for teams in their early stages of training7),(94.
In this context, confirming the findings of other studies that indicated advantages similar to those found in this review2),(89),(95, ISS offers an opportunity to complement the overworked team and compensate for temporary losses due to sick leave or quarantine94.
When performed with planning and coherence, the ISS offers an opportunity to complement technical skills, especially those focused on urgency and emergencies, such as training in trauma care, cardiopulmonary resuscitation (adult and pediatric), actions in the COVID-19 pandemic , sepsis management, birth complications, among others, shown in 114 of the 190 selected articles. In Brazil, the use of ISS was used in scenarios of cardiorespiratory arrest5),(6),(8, sepsis7 and Covid-1996. Regarding the development of non-technical skills, we have as an example its use in promoting patient safety2),(4),(32),(36)-(38),(64),(67),(76)-(79),(97, a safe institutional environment29),(30),(92 and self-management in situations of crisis 18),(57)-(59),(98),(99, of the teams, without the need for travel, without the use of high-cost simulation centers and with a real projection of the participant’s routine. It is noteworthy that ISS is especially important when used in high-risk clinical scenarios with time pressure94.
The use of in situ simulation was also associated with increased clinical reasoning and teamwork capacity, with an overall improvement in the participants’ theoretical practice and practical skills100. When one observes the scenarios in which they were applied, one can associate the findings with other studies that strengthen the obtained data5),(30),(43),(85),(101.
Several articles using ISS to optimize patient safety showed better clarity of team members’ roles in relation to medication administration carried out in the clinical environment95),(102)-(104 and the ability to identify latent safety threats attenuated by practice2),(4),(13),(46),(49),(64)-(70),(76)-(79),(89),(95),(105.
Training programs for multidisciplinary teams4),(11),(12),(22),(32),(39),(53)-(56),(95),(106),(107 using ISS have been shown to effectively improve the technical and non-technical skills of health professionals for managing emergency situations, in addition to optimize learning, both at individual’s and team’s levels90. Thus, ISS can be valuable to improve patient safety, as it allows the practice of care team dynamics within a real clinical environment4.
In simulations in the urgency and emergency sector in the area of pediatrics, studies on training stand out using protocols that showed good performance in work dynamics, such as Pediatric Advanced Life Support (PALS)6),(32),(43.
For Maloney (2018), emergency units favor the use of ISS because they require early identification and management of critical situations by health teams, which must be previously trained for quick and accurate intervention108.
A study with ISS in a pediatric intensive care unit showed a trend towards fewer admissions, a reduction in the morbidity level at the time of admission, a reduction in the length of ICU stay and mortality, which are relevant aspects in the quality of care and patient safety109.
Studies have also shown good results in perinatal care training, significantly improving response times to postpartum hemorrhage in labor and delivery teams with clinical experience, and also decreasing the rate of obstetric trauma and C-section births75),(110.
ISS has also been used to identify and reduce risks during the transport of neonatal patients. One study even promoted changes in transport policy for imaging exams111. Another study showed an improvement in general performance and teamwork in orotracheal intubation in trauma care43.
Studies have also shown success with simulated emergencies in therapies such as extracorporeal membrane oxygenation (ECMO) and the team’s performance during a simulated emergency at the bedside in the coronary unit, making it possible to simulate the invasive procedure necessary to solve the case47),(112.
The COVID-19 pandemic, in fact, was an incentive for a series of transformations, from clinical practice structures, to changes in the implementation of education and research, which required determination, innovation, creativity and adaptability by hospital teams in many circumstances15.
The predominance of ISS applied to multidisciplinary teams demonstrates that it has been used for continuing education, as it leads to greater planning for responses to the complex and growing problems observed in the current context93. Thus, the participants review the relationships between their professions, increase mutual understanding, and explore ways to combine their knowledge to improve service provision, patient safety, and quality of care113.
Although ISS is recognized as a promising field of simulation, unlike the international scenario, where its use is already consolidated in sporadic training programs for health professionals114, few studies are yet identified on the use of this strategy in Brazil5),(6),(96.
It is noteworthy, however, that such results should not be used as evidence for lack of ISS use, as it must be considered that continuing education professionals are not always involved with academia. Thus, there is a hypothesis that its use is not being published in journals, and/or systematically monitored regarding its results. One of the arguments that support this hypothesis is the fact that Mobile Emergency Care Services (SAMU, Serviços de Atendimento Móveis de Urgência) in Brazil have a Permanent Education Center (NEP, Núcleo de Educação Permanente), based on different legislation such as GM Ordinances 2048/02, 1863/03, 198/04, 1996/07, 1010/12, 278/14, among others, which frequently deal with ISS. Nevertheless, it was not possible to identify articles on such training in this review101),(105. Therefore, it would be appropriate to encourage the monitoring of the results of such strategies, and publications to disseminate and increase the level of evidence about their advantages57.
It is worth highlighting the great use of ISS for multidisciplinary training (155/190 articles selected). This strengthens interprofessional collaborative practice which, according to SILVA115, promotes the collective construction of therapeutic projects, sharing of uncertainties, co-accountability of professionals responsible for care and communicative action. The specific actions of each profession involved in health care promote the development of profession-specific skills115.
The sparse use of ISS for the education and training of uniprofessional teams, for example, multiple medical specialties working together (multidisciplinary) is observed.
The training of Swiss physicians based on pediatric simulation (mainly in situ) is a multidisciplinary one, covering technical and non-technical skills and often employing high-tech manikins98.
In Belgium, the use of recurrent training based on in situ simulation had a positive effect on the development of leadership in the neonatal nursing teams; moreover, in this service repeated participation in continuing education in simulation had a positive effect on these results, regardless of the number of years of previous experience58. In the United States of America, regularly scheduled pediatric simulations in the emergency department have resulted in improved staff performance over time in expected resuscitation tasks32.
In Brazil, professionals have observed that the strategy of using in situ simulation as a continuing education tool is valid for professional updating and practical learning in a safe environment5.
Therefore, we recommend the ISS as a useful instrument for training students and health workers at different levels of care and it should be encouraged by managers of health care and education institutions, for practice applied by employees, teachers, students and managers.
A limitation of this study comprises the different characteristics of training and configuration of work teams, as well as the health system of each country, which prevents the generalization of the results.
CONCLUSIONS
The results showed the diverse use of ISS worldwide, demonstrating that its application has grown significantly in recent years. Among the advantages related to ISS, the opportunity to update and acquire knowledge, skills and professional competencies stands out. Its use allowed the improvement in teamwork and individual learning, the ability to offer greater realism and transferability, at a low cost, as it eliminates the high costs of implementing and maintaining a simulation center.
Furthermore, the use of ISS allows an improved performance in real clinical scenarios, helping to reveal important latent risks, and allowing the implementation of corrective measures.
It can be observed that there is still a lot to expand in relation to the use of this resource, especially in Brazil, with regard to the publication of studies and experience reports on this approach. Only five articles published by Brazilian authors were found, applied to urgency and emergency situations in a hospital environment, among the 190 selected for the study.
Therefore, it is suggested that experimental studies be carried out, in different areas of multiprofessional knowledge, to increase evidence on the impact of continuing education using ISS within the characteristics of our country’s education and health systems.
REFERENCES
1. Freund D, Andersen PO, Svane C, Meyhoff CS, Sørensen JL. Unannounced vs announced in situ simulation of emergency teams: feasibility and staff perception of stress and learning. Acta Anaesthesiol Scand. 2019 May;63(5):684-92. [ Links ]
2. Petrosoniak A, Ryzynski A, Lebovic G, Woolfrey K. Cricothyroidotomy in Situ Simulation Curriculum (CRIC Study): training residents for rare procedures. Simul Healthc. 2017 Apr;12(2):76-82. [ Links ]
3. Bloomfield V, Ellis S, Pace J, Morais M. Mode of delivery: development and implementation of an obstetrical in situ simulation program. J Obstet Gynaecol Can. 2020 July;42(7):868-73.e1. [ Links ]
4. Villemure C, Georgescu LM, Tanoubi I, Dubé JN, Chiocchio F, Houle J. Examining perceptions from in situ simulation-based training on interprofessional collaboration during crisis event management in post-anesthesia care. J Interprof Care. 2019 Mar;33(2):182-9. [ Links ]
5. Malfussi LBH, Nascimento ERP, Baptista RCN, Lazzari DD, Martini JG, Hermida PMV. In situ simulation in the permanent education of the intensive care nursing team [Internet]. Texto & Contexto Enferm. 2021;30:e20200130. doi: https://dx.doi.org/10.1590/1980-265x-tce-2020-0130. [ Links ]
6. Kuzma GSP, Hirsch CB, Nau AL, Rodrigues AM, Gubert EM, Soares LCC. Assessment of the quality of pediatric cardiopulmonary resuscitation using the in situ mock code tool. Rev Paul Pediatr. 2020;38:e2018173. doi: https://dx.doi.org/10.1590/1984-0462/2020/38/2018173. [ Links ]
7. Almeida MN, Duarte TTP, Magro MCS. Simulação in situ: ganho da autoconfiança de profissionais de enfermagem na parada cardiopulmonar. Rev Rene. 2019;200:e41535. doi: https://dx.doi.org/10.15253/2175-6783.20192041535. [ Links ]
8. Kaneko RMU, Couto TB, Coelho MM, Taneno AK, Barduzzi NN, Barreto JKS, et al. Simulação in situ, uma metodologia de treinamento multidisciplinar para identificar oportunidades de melhoria na segurança do paciente em uma unidade de alto risco. Rev Bras Educ Med. 2015;39:286-93. doi: https://doi.org/10.1590/1981-52712015v39n2e00242014. [ Links ]
9. Amiel I, Simon D, Merin O, Ziv A. Mobile in situ simulation as a tool for evaluation and improvement of trauma treatment in the emergency department. J Surg Educ. 2016 Jan;73(1):121-8. [ Links ]
10. Lutgendorf MA, Spalding C, Drake E, Spence D, Heaton JO, Morocco KV. Multidisciplinary in situ simulation-based training as a postpartum hemorrhage quality improvement project. Mil Med. 2017;182:e1762-6. [ Links ]
11. Sharara-Chami R, Lakissian Z, Farha R, Tamim H, Batley N. In-situ simulation-based intervention for enhancing teamwork in the emergency department. BMJ Simul Technol Enhanc Learn. 2020;6:175-7. [ Links ]
12. Shrestha A, Sonnenberg T, Shrestha R. Covid-19 emergency department protocols: experience of protocol implementation through in-situ simulation. Open Access Emerg Med. 2020;12:293-303. [ Links ]
13. Jee M, Khamoudes D, Brennan AM, O’Donnell J. Covid-19 outbreak response for an emergency department using in situ simulation. Cureus. 2020;12:e7876. [ Links ]
14. Manggala SK, Tantri AR, Sugiarto A, Sianipar IR, Prasetyono TOH. In situ simulation training for a better interprofessional team performance in transferring critically ill patients with Covid-19: a prospective randomised control trial. Postgrad Med J. 2022;98:617-21. [ Links ]
15. Lateef F, Stawicki SP, Xin LM, Krishnan SV, Sanjan A, Sirur FM, et al. Infection control measures, simulation, and failure modes and effect analysis to fine-tune change management during Covid-19. J Emerg Trauma Shock. 2020;13(4):239-45. doi: https://dx.doi.org/10.4103/jets.jets_119_20. [ Links ]
16. Dharamsi A, Hayman K, Yi S, Chow R, Yee C, Gaylord E, et al. Enhancing departmental preparedness for Covid-19 using rapid-cycle in-situ simulation. J Hosp Infect. 2020;105:604-7. [ Links ]
17. Halls A, Kanagasundaram M, Lau-Walker M, Diack H, Bettles S. Using in situ simulation to improve care of the acutely ill patient by enhancing interprofessional working: a qualitative proof of concept study in primary care in England. BMJ Open. 2019;9:e028572. [ Links ]
18. Sørensen JL, Østergaard D, LeBlanc V. Design of simulation-based medical education and advantages and disadvantages of in situ simulation versus off-site simulation. BMC Med Educ. 2017;17:20. https://doi.org/10.1186/s12909-016-0838-3 [ Links ]
19. Mahankali S, Nair P. Beyond the borders: lessons from various industries adopted in anesthesiology. J Anaesthesiol Clin Pharmacol. 2019;35:295. doi: https://doi.org/10.4103/joacp.joacp_375_18. [ Links ]
20. Pereira Júnior GA, Guedes HTV. Simulação em saúde para ensino e avaliação: conceitos e práticas. ABEM. São Carlos: Cubo Multimídia, 2021. doi: https://doi.org/10.4322/978-65-86819-11-3. [ Links ]
21. Gross B, Rusin L, Kiesewetter J, Zottmann JM, Fischer MR, Prückner S, et al. Crew resource management training in healthcare: a systematic review of intervention design, training conditions and evaluation. BMJ Open . 2019;9:e025247. [ Links ]
22. Patterson MD, Blike GT, Nadkarni VM. In situ simulation: challenges and results. In: Henriksen K, Battles JB, Keyes MA, Grady ML, editors. Advances in patient safety: new directions and alternative approaches. Rockville (MD): Agency for Healthcare Research and Quality; 2008. [ Links ]
23. Araújo ALLS, Quilici AP. O que é simulação e por que simular. In: Quilici AP, Abrão KC, Timermam S, Gutierrez F. Simulação clínica: do conceito à aplicabilidade. São Paulo: Atheneu; 2012. p. 116. [ Links ]
24. Whittemore R, Knafl K. The integrative review: updated methodology. J Adv Nurs. 2005;52(5):546-53. doi: https://dx.doi.org/10.1111/j.1365-2648.2005.03621.x. [ Links ]
25. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLos Med.2009; 6(7):e1000097. doi: https://dx.doi.org/10.1371/journal.pmed.1000097. [ Links ]
26. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan - a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 5;5(1):210. [ Links ]
27. Stetler CB, Morsi D, Rucki S, Broughton S, Corrigan B, Fitzgerald J, et al. Utilization-focused integrative reviews in a nursing service. Appl Nurs Res. 1998;11(4):195-206. doi: https://dx.doi.org/10.1016/s0897-1897(98)80329-7. [ Links ]
28. Bardin L. Análise de conteúdo. São Paulo: Edições 70; 2016. [ Links ]
29. Gignon M, Amsallem C, Ammirati C. Moving a hospital: simulation - a way to co-produce safety healthcare facilities. Int J Occup Saf Ergon. 2017 Dec;23(4):589-91. [ Links ]
30. Argintaru N, Li W, Hicks C, White K, McGowan M, Gray S, et al. An active shooter in your hospital: a novel method to develop a response policy using in situ simulation and video framework analysis. Disaster Med Public Health Prep. 2021;15(2):223-31. doi: https://dx.doi.org/10.1017/dmp.2019.161. [ Links ]
31. Mustafa M, Lutfi R, Alsaedi H, Castelluccio P, Pearson KJ, Montgomery EE, et al. Improvement of pediatric advanced airway management in general emergency departments after a collaborative intervention program. Respir Care. 2021;66:1866-75. [ Links ]
32. Katznelson JH, Wang J, Stevens MW, Mills WA. Improving pediatric preparedness in critical access hospital emergency departments: impact of a longitudinal in situ simulation program. Pediatr Emerg Care. 2018;34:17-20. [ Links ]
33. Barni S, Mori F, Giovannini M, Luca M de, Novembre E. In situ simulation in the management of anaphylaxis in a pediatric emergency department. Intern Emerg Med. 2019;14:127-32. [ Links ]
34. Surcouf JW, Chauvin SW, Ferry J, Yang T, Barkemeyer B. Enhancing residents’ neonatal resuscitation competency through unannounced simulation-based training. Med Educ Online. 2013;18:1-7. [ Links ]
35. Abu-Sultaneh S, Whitfill T, Rowan CM, Friedman ML, Pearson KJ, Berrens ZJ, et al. Improving simulated pediatric airway management in community emergency departments using a collaborative program with a pediatric academic medical center. Respir Care . 2019;64:1073-81. [ Links ]
36. Lee C, Mowry JL, Maycock SE, Colaianne-Wolfer ME, Knight SW, Wyse DM. The impact of hospital-based in situ simulation on nurses’ recognition and intervention of patient deterioration. J Nurses Prof Dev. 2019;35:18-24. [ Links ]
37. Abulebda K, Whitfill T, Montgomery EE, Kirby ML, Ahmed RA, Cooper DD, et al. Improving pediatric diabetic ketoacidosis management in community emergency departments using a simulation-based collaborative improvement program. Pediatr Emerg Care . 2021 Nov 1;37(11):543-9. doi: https://doi.org/10.1097/PEC.0000000000001751. [ Links ]
38. Saqe-Rockoff A, Ciardiello AV, Schubert FD. Low-fidelity, in-situ pediatric resuscitation simulation improves RN Competence and self-efficacy. J Emerg Nurs. 2019;45:538-44.e1. [ Links ]
39. Rubio-Gurung S, Putet G, Touzet S, Gauthier-Moulinier H, Jordan I, Beissel A, et al. In situ simulation training for neonatal resuscitation: an RCT. Pediatrics. 2014;134:e790-7 [ Links ]
40. Adcock S, Kuszajewski ML, Dangerfield C, Muckler VC. Optimizing nursing response to in-hospital cardiac arrest events using in situ simulation. Clin Simul Nurs. 2020;49:16-8. [ Links ]
41. Whitfill T, Gawel M, Auerbach M. A Simulation-based quality improvement initiative improves pediatric readiness in community hospitals. Pediatr Emerg Care . 2018;34:431-5. [ Links ]
42. Arul N, Ahmad I, Hamilton J, Sey R, Tillson P, Hutson S, et al. Lessons learned from a collaborative to develop a sustainable simulation-based training program in neonatal resuscitation: simulating success. Children. 2021;8(1):39. doi: https://doi.org/10.3390/children8010039. [ Links ]
43. Auerbach M, Roney L, Aysseh A, Gawel M, Koziel J, Barre K, et al. In situ pediatric trauma simulation: assessing the impact and feasibility of an interdisciplinary pediatric in situ trauma care quality improvement simulation program. Pediatr Emerg Care . 2014 Dec;30(12):884-91. [ Links ]
44. Wong KU, Gross I, Emerson BL, Goldman MP. Simulated airway drills as a tool to measure and guide improvements in endotracheal intubation preparation in the paediatric emergency department. BMJ Simul Technol Enhanc Learn . 2021;7:561-7. [ Links ]
45. Bayouth L, Ashley S, Brady J, Lake B, Keeter M, Schiller D, et al. An in-situ simulation-based educational outreach project for pediatric trauma care in a rural trauma system. J Pediatr Surg. 2018;53:367-71. [ Links ]
46. Gros E, Shi R, Hasty B, Anderson T, Schmiederer I, Roman-Micek T, et al. In situ interprofessional operating room simulations: empowering learners in crisis resource management principles. Surgery. 2021;170:432-9. [ Links ]
47. Chan SY, Figueroa M, Spentzas T, Powell A, Holloway R, Shah S. Prospective assessment of novice learners in a simulation-based Extracorporeal Membrane Oxygenation (ECMO) education program. Pediatr Cardiol. 2013;34:543-52. doi: https://dx.doi.org/10.1007/s00246-012-0490-6. [ Links ]
48. Calhoun AW, Boone MC, Dauer AK, Campbell DR, Montgomery VL. Using simulation to investigate the impact of hours worked on task performance in an intensive care unit. Am J Crit Care. 2014;23:387-95. [ Links ]
49. Uttley E, Suggitt D, Baxter D, Jafar W. Multiprofessional in situ simulation is an effective method of identifying latent patient safety threats on the gastroenterology ward. Frontline Gastroenterol. 2020;11:351-7. [ Links ]
50. Bullough AS, Wagner S, Boland T, Waters TP, Kim K, Adams W. Obstetric team simulation program challenges. J Clin Anesth. 2016;35:564-70. [ Links ]
51. Clapper TC, Lee J, Phillips J, Rajwani K, Naik N, Ching K. Gibson’s theory of affordances and situational awareness occurring in urban departments of pediatrics, medicine, and emergency medicine. Educ Health. 2018;31:87-94. [ Links ]
52. Shi R, Marin-Nevarez P, Hasty B, Roman-Micek T, Hirx S, Anderson T, et al. Operating room in situ interprofessional simulation for improving communication and teamwork. J Surg Res. 2021;260:237-44. [ Links ]
53. Jonsson K, Brulin C, Härgestam M, Lindkvist M, Hultin M. Do team and task performance improve after training situation awareness? A randomized controlled study of interprofessional intensive care teams. Scand J Trauma Resusc Emerg Med. 2021;29:73. [ Links ]
54. Dryver E, Knutsson J, Ekelund U, Bergenfelz A. Impediments to and impact of checklists on performance of emergency interventions in primary care: an simulation-based randomized controlled trial. Scand J Prim Health Care. 2021;39:438-47. [ Links ]
55. Eckels M, Zeilinger T, Lee HC, Bergin J, Halamek LP, Yamada N, et al. A Neonatal intensive care unit’s experience with implementing an in-situ simulation and debriefing patient safety program in the setting of a quality improvement collaborative. Children . 2020;7(11):202. doi: https://doi.org/10.3390/children7110202. [ Links ]
56. Qian J, Wang Y, Zhang Y, Zhu X, Rong Q, Wei H. A survey of the first-hour basic care tasks of severe sepsis and septic shock in pediatric patients and an evaluation of medical simulation on improving the compliance of the tasks. J Emerg Med. 2016;50:239-45. [ Links ]
57. Monette DL, Hegg DD, Chyn A, Gordon JA, Takayesu JK. A guide for medical educators: how to design and implement in situ simulation in an academic emergency department to support interprofessional education. Cureus . 2021 May;13(5):e14965. doi: https://dx.doi.org/10.7759/cureus.14965. [ Links ]
58. Maenhout G, Billiet V, Sijmons M, Beeckman D. The effect of repeated high-fidelity in situ simulation-based training on self-efficacy, self-perceived leadership qualities and team performance: a quasi-experimental study in a NICU-setting. Nurse Educ Today. 2021;100:104849. [ Links ]
59. Jonsson K, Brulin C, Härgestam M, Lindkvist M, Hultin M. Do team and task performance improve after training situation awareness? A randomized controlled study of interprofessional intensive care teams. Scand J Trauma Resusc Emerg Med . 2021;29:73. [ Links ]
60. Rød I, Kynø NM, Solevåg AL. From simulation room to clinical practice: postgraduate neonatal nursing students’ transfer of learning from in-situ resuscitation simulation with interprofessional team to clinical practice. Nurse Educ Pract. 2021;52:102994. [ Links ]
61. Monesi A, Imbriaco G, Mazzoli CA, Giugni A, Ferrari P. In-situ simulation for intensive care nurses during the Covid-19 pandemic in Italy: advantages and challenges. Clin Simul Nurs . 2022 Jan;62:52-6. [ Links ]
62. Contreras M, Curran E, Ross M, Moran P, Sheehan A, Brennan AM, et al. Rapid development of interprofessional in situ simulation-based training in response to the Covid-19 outbreak in a tertiary-level hospital in Ireland: initial response and lessons for future disaster preparation. BMJ Simul Technol Enhanc Learn . 2021;7:159-62. [ Links ]
63. Earle D, Betti D, Scala E. Development of a rapid response plan for intraoperative emergencies: the circulate, scrub, and technical assistance team. Am J Surg. 2017;213:181-6. [ Links ]
64. Barbeito A, Bonifacio A, Holtschneider M, Segall N, Schroeder R, Mark J, et al. In situ simulated cardiac arrest exercises to detect system vulnerabilities. Simul Healthc . 2015;10:154-62. [ Links ]
65. Biddell EA, Vandersall BL, Bailes SA, Estephan SA, Ferrara LA, Nagy KM, et al. Use of simulation to gauge preparedness for ebola at a free-standing children’s hospital. Simul Healthc 2016;11:94-9. [ Links ]
66. Shah SJ, Cusumano C, Ahmed S, Ma A, Jafri FN, Yang CJ. In situ simulation to assess pediatric tracheostomy care safety: a novel multicenter quality improvement program. Otolaryngol Head Neck Surg. 2020 Aug;163(2):250-8. doi: https://doi.org/10.1177/0194599820923659. [ Links ]
67. Kalidindi S, Kirk M, Griffith E. In-situ simulation enhances emergency preparedness in pediatric care practices. Cureus . 2018 Oct 1º;10(10):e3389. doi: https://doi.org /10.7759/cureus.3389. [ Links ]
68. Chima AM, Koka R, Lee B, Tran T, Ogbuagu OU, Nelson-Williams H, et al. Medical simulation as a vital adjunct to identifying clinical life-threatening gaps in austere environments. J Natl Med Assoc. 2018;110:117-23. [ Links ]
69. Yager P, Collins C, Blais C, O’Connor K, Donovan P, Martinez M, et al. Quality improvement utilizing in-situ simulation for a dual-hospital pediatric code response team. Int J Pediatr Otorhinolaryngol. 2016;88:42-6. [ Links ]
70. Sørensen JL, Lottrup P, Vleuten C van der, Andersen KS, Simonsen M, Emmersen P, et al. Unannounced in situ simulation of obstetric emergencies: staff perceptions and organisational impact. Postgrad Med J . 2014 Nov;90(1069):622-9. [ Links ]
71. Hinde T, Gale T, Anderson I, Roberts M, Sice P. A study to assess the influence of interprofessional point of care simulation training on safety culture in the operating theatre environment of a university teaching hospital. J Interprof Care . 2016;30:251-3. [ Links ]
72. Brown KM, Mudd SS, Perretta JS, Dodson A, Hunt EA, McMillan KN. Rapid cycle deliberate practice to facilitate “nano” in situ simulation: an interprofessional approach to just-in-time training. Crit Care Nurse. 2021;41:e1-8. [ Links ]
73. Schram A, Paltved C, Christensen KB, Kjaergaard-Andersen G, Jensen HI, Kristensen S. Patient safety culture improves during an in situ simulation intervention: a repeated cross-sectional intervention study at two hospital sites. BMJ Open Qual. 2021;10:e001183. doi: https://doi.org/10.1136/bmjoq-2020-001183. [ Links ]
74. Kessler DO, Walsh B, Whitfill T, Dudas RA, Gangadharan S, Gawel M, et al. Disparities in adherence to pediatric sepsis guidelines across a spectrum of emergency departments: a multicenter, cross-sectional observational in situ simulation study. J Emerg Med . 2016;50:403-15.e1-3. [ Links ]
75. Kahwati LC, Sorensen AV, Teixeira-Poit S, Jacobs S, Sommerness SA, Miller KK, et al. Impact of the agency for healthcare research and quality’s safety program for perinatal care. Jt Comm J Qual Patient Saf. 2019 Apr;45(4):231-40. [ Links ]
76. Fan M, Petrosoniak A, Pinkney S, Hicks C, White K, Almeida APSS, et al. Study protocol for a framework analysis using video review to identify latent safety threats: trauma resuscitation using in situ simulation team training (TRUST). BMJ Open . 2016;6:e013683. [ Links ]
77. Gupta N, Sones A, Powell M, Robbins J, Wilson S, Hill A, et al. Quality improvement methodology to optimize safe early mobility in a pediatric intensive care unit. Pediatr Qual Saf. 2021;6:e369. doi: https://dx.doi.org/10.1097/pq9.0000000000000369. [ Links ]
78. Phitayakorn R, Levine W, Petrusa E, Daily B, Eromo E, Gee D, et al. Making it real: development and integration of in situ simulation operating rooms into the real operating room environment. IEEE Pulse. 2015;6:10-3. [ Links ]
79. Gangadharan S, Tiyyagura G, Gawel M, Walsh BM, Brown LL, Lavoie M, et al. A grounded theory qualitative analysis of interprofessional providers’ perceptions on caring for critically ill infants and children in pediatric and general emergency departments. Pediatr Emerg Care . 2018;34:578-83. [ Links ]
80. Nadir NA, Kim J, Cassara M, Hrdy M, Zaveri P, Wong AH, et al. Simulation-based emergency medicine education in the era of physical distancing. AEM Educ Train. 2021;5:e10586. [ Links ]
81. Hall A, Kawai K, Graber K, Spencer G, Roussin C, Weinstock P, et al. Acoustic analysis of surgeons’ voices to assess change in the stress response during surgical in situ simulation. BMJ Simul Technol Enhanc Learn . 2021;7:471-7. [ Links ]
82. Kurosawa H, Ikeyama T, Achuff P, Perkel M, Watson C, Monachino A, et al. A randomized, controlled trial of in situ Pediatric Advanced Life Support recertification (“Pediatric Advanced Life Support reconstructed”) compared with standard Pediatric Advanced Life Support recertification for ICU frontline providers. Crit Care Med. 2014;42:610-8. [ Links ]
83. Bredmose PP, Hagemo J, Østergaard D, Sollid S. Combining in-situ simulation and live HEMS mission facilitator observation: a flexible learning concept. BMC Med Educ . 2021;21:579. [ Links ]
84. Meerdink M, Khan J. Comparison of the use of manikins and simulated patients in a multidisciplinary in situ medical simulation program for healthcare professionals in the United Kingdom. J Educ Eval Health Prof. 2021;18:8. [ Links ]
85. George KL, Quatrara B. Interprofessional simulations promote knowledge retention and enhance perceptions of teamwork skills in a surgical-trauma-burn intensive care unit setting. Dimens Crit Care Nurs. 2018;37:144-55. [ Links ]
86. Brogaard L, Hvidman L, Hinshaw K, Kierkegaard O, Manser T, Musaeus P, et al. Development of the TeamOBS-PPH - targeting clinical performance in postpartum hemorrhage. Acta Obstet Gynecol Scand. 2018;97:677-87. [ Links ]
87. Vail B, Spindler H, Morgan MC, Cohen SR, Christmas A, Sah P, et al. Care of the mother-infant dyad: a novel approach to conducting and evaluating neonatal resuscitation simulation training in Bihar, India. BMC Pregnancy Childbirth. 2017;17:252. [ Links ]
88. Saqe-Rockoff A, Ciardiello AV, Schubert FD. Low-Fidelity, In-Situ Pediatric Resuscitation Simulation Improves RN Competence and Self-Efficacy. J Emerg Nurs . 2019;45:538-44.e1. [ Links ]
89. Lavelle M, Attoe C, Tritschler C, Cross S. Managing medical emergencies in mental health settings using an interprofessional in-situ simulation training programme: a mixed methods evaluation study. Nurse Educ Today . 2017 Dec;59:103-9. [ Links ]
90. Rollison S, Blessing R, Kuszajewski ML, Muckler VC. In situ simulation to improve management of in-hospital strokes: unexpected challenges. Clin Simul Nurs . 2018;24:30-4. doi: https://dx.doi.org/10.1016/j.ecns.2018.09.004. [ Links ]
91. Fregene TE, Nadarajah P, Buckley JF, Bigham S, Nangalia V. Use of in situ simulation to evaluate the operational readiness of a high-consequence infectious disease intensive care unit. Anaesthesia. 2020;75(6):733-8. doi: https://dx.doi.org/10.1111/anae.15048. [ Links ]
92. Carmichael H, Mastoras G, Nolan C, Tan H, Tochkin J, Poulin C, et al. Integration of in situ simulation into an emergency department code orange exercise in a tertiary care trauma referral center. AEM Educ Train. 2021 Apr;5(2):e10485. doi: https://dx.doi.org/10.1002/aet2. [ Links ]
93. Frenk J, Chen L. Transforming health professionals’ education - authors’ reply. Lancet. 2011;377(9773):1238-9. doi: https://dx.doi.org/10.1016/s0140-6736(11)60500-x. [ Links ]
94. Kalnow A, Davis A, Hampton Z, Gable BD. In situ simulation to promote residents as resuscitation leaders. Cureus . 2021 Apr;13(4):e14449. [ Links ]
95. Dale-Tam J, McBride K. My throat is itchy! An in-situ simulation for interprofessional healthcare education. Cureus . 2019 Apr 2;11(4):e4366. doi: https://dx.doi.org/10.7759/cureus.4366. [ Links ]
96. Santos TM, Pedrosa RBS, Carvalho DRS, Franco MH, Silva JLG, Franci D, et al. Implementing healthcare professionals’ training during Covid-19: a pre and post-test design for simulation training. Sao Paulo Med J. 2021 May;139(5):514-9. doi: https://doi.org/10.1590/1516-3180.2021.0190.R1.27052021. [ Links ]
97. Kjaergaard-Andersen G, Ibsgaard P, Paltved C, Irene Jensen H. An in situ simulation program: a quantitative and qualitative prospective study identifying latent safety threats and examining participant experiences. Int J Qual Health Care. 2021;33. doi: https://doi.org/10.1093/intqhc/mzaa148. [ Links ]
98. Stocker M, Laine K, Ulmer F. Use of simulation-based medical training in Swiss pediatric hospitals: a national survey. BMC Med Educ . 2017 June 17;17(1):104. doi: https://doi.org/10.1186/s12909-017-0940-1. [ Links ]
99. Kerner RL, Gallo K, Cassara M, D'Angelo J, Egan A, Simmons JG. Simulation for operational readiness in a new freestanding emergency department: strategy and tactics. Simul Healthc . 2016 Oct;11(5):345-356. doi: https://doi.org/10.1097/SIH.0000000000000180. [ Links ]
100. Wang W, Han C, Zhang X, Tong Y, Zhao R, Wang B, et al. Application of in situ simulation teaching in the training of trainee nurses to respond to emergencies. Ann Palliat Med. 2021 Apr;10(4):4509-15. [ Links ]
101. Soares GSD, Azevedo CRF de. Simulação clínica como estratégia de implementação de educação permanente em Serviço de Atendimento Móvel de Urgência. Rev Chronos Urg. 2022;1(1):e1121.25 [acesso em 6 jul 2021]. Dosponível: Dosponível: https://chronos.samu.fortaleza.ce.gov.br/index.php/urgencia/article/view/25 . [ Links ]
102. Rusiecki D, Walker M, Douglas SL, Hoffe S, Chaplin T. Multiprofessional perspectives on the identification of latent safety threats via in situ simulation: a prospective cohort pilot study. BMJ Simul Technol Enhanc Learn . 2021;7:102-7. [ Links ]
103. Rozenfeld RA, Nannicelli AP, Brown AR, Eppich WJ, Woods DM, Lestrud SO, et al. Verbal communication during airway management and emergent endotracheal intubation: observations of team behavior among multi-institutional pediatric intensive care unit in situ simulations. J Patient Saf. 2020;16:e114-9. [ Links ]
104. Jones MD, McGrogan A, Raynor DK, Watson MC, Franklin BD. User-testing guidelines to improve the safety of intravenous medicines administration: a randomised in situ simulation study. BMJ Qual Saf. 2021;30:17-26. [ Links ]
105. Gable BD, Hommema L. In-situ simulation in interdisciplinary family practice improves response to in-office emergencies. Cureus . 2021Apr 6;13(4):e14315. doi: https://dx.doi.org/10.7759/cureus.14315. [ Links ]
106. Benlolo S, Nensi A, Campbell DM, Assouad C, Taylor TS, Shore EM. The use of in situ simulation to enhance Covid-19 pandemic preparedness in obstetrics. Cureus . 2021;13:e12906. [ Links ]
107. Siegel NA, Kobayashi L, Dunbar-Viveiros JA, Devine J, Al-Rasheed RS, Gardiner FG, et al. In situ medical simulation investigation of emergency department procedural sedation with randomized trial of experimental bedside clinical process guidance intervention. Simul Healthc . 2015;10:146-53. [ Links ]
108. Maloney A, Field PE. In situ simulation training for management of emergency situations and deteriorating patients in GP surgeries. BMJ Simul Technol Enhanc Learn . 2018;4(2): A32-A33. doi: https://dx.doi.org/10.1136/bmjstel-2018-aspihconf.60. [ Links ]
109. Theilen U, Leonard P, Jones P, Ardill R, Weitz J, Agrawal D, et al. Regular in situ simulation training of paediatric medical emergency team improves hospital response to deteriorating patients. Resuscitation. 2013 Feb;84(2):218-22. [ Links ]
110. Marshall NE, Vanderhoeven J, Eden KB, Segel SY, Guise JM. Impact of simulation and team training on postpartum hemorrhage management in non-academic centers. J Matern Fetal Neonatal Med. 2015 Mar;28(5):495-9. [ Links ]
111. Wong J, Kalaniti K, Castaldo M, Whyte H, Lee KS, Schroff M, et al. Utilizing simulation to identify latent safety threats during neonatal magnetic resonance imaging procedure. Simul Healthc . 2021 June 1º;16(3):170-6. [ Links ]
112. Hamilton AJ, Prescher H, Biffar DE, Poston RS. Simulation trainer for practicing emergent open thoracotomy procedures. J Surg Res . 2015 July;197(1):78-84. [ Links ]
113. World Health Organization. Framework for action on interprofessional education & collaborative practice. Geneva: WHO; 2010. [ Links ]
114. Wilson L, Farooq O. Fire in operating theatres: DaSH-ing to the rescue. J Perioper Pract. 2018;(7):188-93. [ Links ]
115. Silva JAM, Peduzzi M, Orchard C, Leonello VM. Educação interprofissional e prática colaborativa na Atenção Primária à Saúde. Rev Esc Enferm USP. 2015;49(1):16-24. doi: https://dx.doi.org/10.1590/s0080-623420150000800003. [ Links ]
Received: January 25, 2023; Accepted: October 02, 2023











 texto em
texto em 



