Serviços Personalizados
Journal
Artigo
Compartilhar
Revista Brasileira de Educação Médica
versão impressa ISSN 0100-5502versão On-line ISSN 1981-5271
Rev. Bras. Educ. Med. vol.48 no.4 Rio de Janeiro 2024 Epub 19-Nov-2024
https://doi.org/10.1590/1981-5271v48.4-2024-0059
ORIGINAL ARTICLE
Impact of an educational intervention on patient safety for anesthesiology residents
1 Universidade Federal do Rio Grande do Norte, Maternidade Escola Januário Cicco, Programa de Pós-Graduação em Ensino em Saúde, Natal, Rio Grande do Norte, Brasil.
2 Universidade Federal do Rio Grande do Norte, Natal, Rio Grande do Norte, Brasil.
3 Universidade Federal do Rio Grande do Norte, Hospital Universitário Onofre Lopes, Natal, Rio Grande do Norte, Brasil.
4 Universidade Federal do Rio Grande do Norte, Programa de Pós-Graduação em Ensino na Saúde, Natal, Rio Grande do Norte, Brasil.
Introduction:
The competency matrix of the Medical Residency Programs in Anesthesiology in Brazil has as its specific objective “performing anesthesia safely in all its stages”, whose elements for the implementation of a specific curriculum need to be defined. Given this scenario, the development and implementation of an educational module on patient safety for anesthesiology residents has been proposed.
Objective:
To develop and implement an educational module on patient safety in anesthesiology for residents in the specialty and to evaluate the module effectiveness and the residents’ degree of satisfaction with it.
Method:
A quasi-experimental study with an interrupted time series design with a group was carried out within the scope of the professional master’s degree in health education, at a public university in northeastern Brazil, with anesthesiology residents attending the three years of the residency program. An educational module was developed in e-book format, and a pedagogical strategy was implemented to mediate the residents’ learning in four face-to-face meetings, held during practical activities at the hospital. A pre-test knowledge assessment was performed before the first discussion of patient safety content at the first meeting, and a post-test at the last meeting, and satisfaction assessment was performed using a Likert scale questionnaire.
Results:
Pre-test scores ranged from 6.25 to 8.75 (mean 7.50), while post-test scores ranged from 7.50 to 10.0 (mean 9.03). There was a significant improvement in the median scores in the post-test from 7.50 to 8.75, with p = 0.0199. The satisfaction questionnaire (Cronbach’s alpha coefficient = 0.793) showed satisfactory responses for each of the items evaluated, all ranging from “I agree” to “I fully agree”.
Conclusion:
The development and implementation of an educational module to mediate learning during the training process of anesthesiology residents were effective in promoting knowledge about patient safety for anesthesiologists in training, with high satisfaction rates. Therefore, we emphasize the importance of including the topic of patient safety in the curricular structure of anesthesiology residency courses, with protected space and time for these professionals’ learning process. Moreover, further studies are needed to measure the long-term impact of this intervention, its influence on the acquisition of skills, and whether these educational interventions improve patient outcomes.
Keywords: Patient Safety; Anesthesiology; Medical Residency; Curriculum
Introdução:
A matriz de competências dos programas de residência médica em anestesiologia do Brasil apresenta como objetivo específico “realizar a anestesia com segurança em todas as suas etapas”, cujos elementos para a implementação de um currículo específico precisam ser definidos. Diante desse cenário, foram propostas a elaboração e a implementação de um módulo educacional sobre segurança do paciente para residentes de anestesiologia.
Objetivo:
Este estudo teve como objetivos desenvolver e implementar um módulo educacional sobre segurança do paciente em anestesiologia para residentes da especialidade, e avaliar a efetividade e o grau de satisfação deles com o módulo.
Método:
Trata-se de um estudo quase experimental com desenho série temporal interrompida com um grupo, realizado no âmbito do mestrado profissional em Ensino na Saúde, de uma universidade pública do Nordeste do Brasil, com residentes de anestesiologia dos três anos. Desenvolveu-se um módulo educacional, em formato e-book, e implementou-se uma estratégia pedagógica para intermediar a aprendizagem de residentes, em quatro encontros presenciais, ocorridos durante o expediente de atividades práticas no hospital. Realizaram-se uma avaliação de conhecimentos com pré-teste, antes da primeira discussão dos conteúdos de segurança do paciente, no primeiro encontro, e pós-teste, no último encontro, e uma avaliação de satisfação utilizando questionário com escala Likert.
Resultado:
As notas do pré-teste variaram de 6.25 a 8.75 (média 7.50), enquanto no pós-teste houve uma variação de 7.50 a 10.0 (média 9.03). Houve melhora significativa das notas medianas no pós-teste de 7.50 para 8.75, com p = 0.0199. O questionário de satisfação (coeficiente alfa de Cronbach = 0.793) apresentou respostas satisfatórias para cada um dos itens avaliados, todas variando de “concordo” a “concordo totalmente”.
Conclusão:
A elaboração e implementação de um módulo educacional para intermediar a aprendizagem durante o processo formativo de residentes de anestesiologia foram efetivas em promover conhecimento sobre segurança do paciente para o anestesiologista em formação, com altos índices de satisfação. Assim, ressalta-se a importância da inserção do tema segurança do paciente na estrutura curricular dos cursos de residência em anestesiologia, com espaço e tempo protegidos para o processo de aprendizagem desses profissionais. Ademais, são necessários mais estudos que possam mensurar o impacto dessa intervenção em longo prazo, sua influência na aquisição de competências e se essas intervenções educacionais melhoram os resultados para os pacientes.
Palavras-chave: Segurança do Paciente; Anestesiologia; Residência Médica; Currículo
INTRODUCTION
Anesthesiology is a medical specialty recognized for its associated risks and for its constant concern with improvements in the field of patient safety (PS). Anesthesiologists are involved in the care of a large number of patients, whose work takes place in complex systems involving procedures with several critical steps, professionals with different training, use of equipment, drugs, techniques and technologies, which requires a high level of vigilance. These factors, added to the constant increase in the complexity of surgical procedures, the growing pressure for productivity and results, high workload, lack of control over the schedule and issues related to the high risk of mental exhaustion, represent a greater risk for failures and potential injuries to patients undergoing anesthesia.
A robust education on PS, especially during the training phase of new professionals, is a demand of the National Patient Safety Program (PNSP, Programa Nacional de Segurança do Paciente)1 and the Declaration of Helsinki2 on patient safety in anesthesiology, which highlights that “Education has a fundamental role in improving safety, and we fully support the development, dissemination and training in patient safety.”
The competency matrix of the Medical Residency Programs in Anesthesiology in Brazil also has objectives related to training in PS3. The matrix is the result of the change from a traditional curriculum based on training time to a competency-based curriculum. Mandatory since March 1, 2020, the competency matrix has as its specific objective “To perform anesthesia safely in all its stages” and other objectives related to the stratification and reduction of anesthetic-surgical risk3.
Despite this, however, there is no clear definition of what the curriculum on patient safety in anesthesiology should be like, and it is up to the residency program to structure its method of teaching on the subject using the available resources4. Studies that evaluated the performance of anesthesiology residents on the subject showed low performance, which was attributed to the lack of more in-depth and effective knowledge, appreciation of the subject and ineffective teaching5. Additionally, physicians in specialization constitute a population of health professionals who are vulnerable in terms of patient safety due to their lack of experience and knowledge on the subject. This, combined with their workload and competing learning priorities, potentially places these physicians and their patients at increased risk of involvement in adverse events6.
Considering this scenario, this study aims to train Anesthesiology residents on safe practices that are of great relevance to minimize incidents related to the care of patients undergoing anesthesia. For this purpose, the objective was to develop and implement an educational module on patient safety in anesthesiology for residents in the specialty and to evaluate the module effectiveness and the residents’ degree of satisfaction with it.
METHOD
This is a study with a quasi-experimental design and interrupted time series design with a group7, carried out within the scope of the professional Master’s Degree in health education, at Universidade Federal do Rio Grande do Norte - UFRN, with 10 residents attending from the first to the third year of the Medical Residency Program in Anesthesiology at the Onofre Lopes University Hospital, which belongs to the Brazilian Company of Hospital Services (Ebserh - Empresa Brasileira de Serviços Hospitalares) network. The study was developed in two stages, the first being the creation of the educational module entitled “Patient Safety in the Anesthesiologist’s Practice”, in the e-book format with eight units, as shown in Chart 1:
Chart 1 Contents of the e-book “Patient Safety in the Anesthesiologist’s Practice”.
| Patient Safety in the Anesthesiologist’s Practice | |
|---|---|
| Unit 1: Health Safety - concept, history and taxonomy | It presents basic concepts and structuring aspects of patient safety (PS) and a brief history8 of PS in Brazil and in the world and discusses key terms. |
| Unit 2: Safety Culture and the Complexity of Health Systems | It addresses information that contributes to the understanding, promotion and maintenance of a safety culture; complex systems and their relationship with the anesthesiologist’s work environment; and the appropriate approach to error. |
| Unit 3: Safe Surgery Saves Lives and WHO Surgical Safety Checklist | It presents adverse events in surgical procedures: morbidity and mortality and impact on public health9; the importance and main items of the WHO Surgical Checklist and its application, including correct patient identification. |
| Unit 4: Anesthetic System Verification | Highlights the essential verification items for carrying out the anesthetic act and its regulation9),(10. |
| Unit 5: Surgical Site Infection Prevention. | It addresses hand hygiene as a component of infection prevention and control12),(13; the role of the anesthesiologist in preventing healthcare-related infections, especially surgical site infections. |
| Unit 6: Safety in drug administration | Presents anesthesiology as a specialty with a significant risk of drug-related errors; safe practices to prevent adverse events related to incorrect drug administration14),(15. |
| Unit 7: Adverse events related to airway management | Discusses the importance of adequate airway management to minimize/prevent adverse events; difficult airway management strategies according to updated guidelines16),(17),(18),(19),(20),(21. |
| Unit 8: Prevention of falls and injuries caused by the positioning of the patient under anesthesia16),(17), (22),(23),(24. | Discusses the risk of falls in patients undergoing anesthesia; the physiological changes and risks of harm to the patient associated with each type of positioning on the surgical table; the most appropriate practices for patient positioning. |
Source: prepared by the authors.
During the second stage, the educational module was applied and residents were assessed, organized in four face-to-face meetings, with the participation of 10 residents (three, four and three residents attending the first, second and third years of residency, respectively). In the first meeting, the participants answered a pre-test questionnaire to assess prior knowledge, which was available online, consisting of eight multiple-choice questions, with each question corresponding to one Unit of the e-book.
Also in the first meeting, the educational module was made available to participants in PDF e-book format and an introductory lecture was held on the general aspects of the topic of PS and safety culture, corresponding to Units 1 and 2 of the e-book. It was established that at each subsequent meeting (with one-week intervals), after the participants had previously read the content individually, two Units of the educational module would be presented in person at the hospital where the residency was held, through the discussion of published clinical cases, resolution and discussion of questions prepared by the Teaching and Training Committee of the Brazilian Society of Anesthesiology (SBA, Sociedade Brasileira de Anestesiologia) between 2015 and 2022, and the sharing of the residents’ experiences. Thus, this pedagogical strategy was maintained in the following meetings.
At the end of the fourth and final meeting, in addition to the presentation and discussion of the module’s content, two types of questionnaires were applied: the first to assess the knowledge acquired through a post-test instrument similar to the pre-test one and the second related to the satisfaction assessment questionnaire.
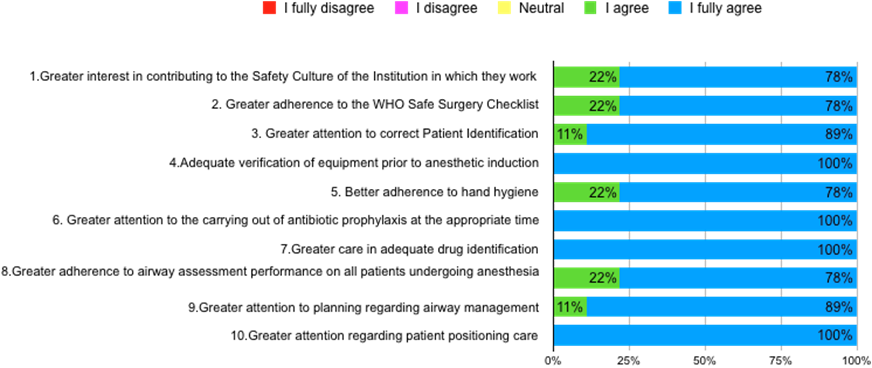
The satisfaction questionnaire was made available online and included 18 questions, organized into two parts: in the first, the participants answered six questions about their satisfaction with the course structure (content, language, format, organization and acquisition of knowledge) and the following open-ended question: “Would you recommend other topics that you consider important for the discussion on patient safety in the practice of anesthesiology and that were not covered by the teaching material?”.
In the second, the participants self-assessed their perception of the impact that the knowledge acquired through the educational intervention could have on their clinical practice. The assessed items are related to the objectives of each discussed topic, such as: greater interest in contributing to the safety culture; adherence to the World Health Organization (WHO) Safe Surgery Checklist; patient identification; adequate verification of equipment before anesthetic induction; hand hygiene; administration of antibiotic prophylaxis at the appropriate time; adequate drug identification; performing an airway assessment of all patients undergoing anesthesia; planning the airway approach; greater attention to patient positioning care.
In addition, at the end of this section there was a space for criticism, suggestions or praise of the teaching material presented, which was not mandatory.
A five-point Likert scale was used, which included I Fully Disagree = 1; I Disagree = 2; Neutral = 3; I Agree = 4 and I Fully Agree = 5, for the closed questions in both parts of the questionnaire. To estimate the satisfaction questionnaire reliability, the Cronbach’s alpha coefficient value was calculated (analysis performed using the R programming language - R CORE TEAM, 2023)25, with the 16 questions of the questionnaire in which the Likert Scale was used.
Regarding data analysis, the categorical data were represented in tables using frequencies and their respective percentages. Measures such as minimum value, median, mean, standard deviation and maximum value were used to represent the quantitative data. To analyze the pre- and post-test questionnaires, the students’ final grades in the pre- and post-test were compared, assessing whether the grades showed a significant difference, using the t-test and Wilcoxon test. The Shapiro-Wilk test was also used to test the normality of the data. The level of significance adopted was α = 5%. All analyses were performed using the R25 programming language (R CORE TEAM, 2023). Finally, the responses to the Satisfaction Questionnaire were evaluated and summarized in a table with the distribution of the general data and by year of residency, as well as their respective percentages.
The study was approved by the Research Ethics Committee (REC) of the institution under CAAE number 60774022.2.0000.5292 and all residents involved in the study signed the Free and Informed Consent Form.
RESULTS
1- Pre and post-test knowledge assessment
Ten residents (three from the 1st year, four from the 2nd year and three from the 3rd year of residency) participated in the training activity; however, nine completed the pre- and post-tests. The pre-test scores ranged from 6.25 to 8.75, while in the post-test they ranged from 7.50 to 10.0, with averages of 7.50 and 9.03 respectively (Table 1), with a significant difference for the values of the median scores in the two moments of test application through the Wilcoxon test.
Table 1 Comparison of pre- and post-test scores obtained by residents.
| Metrics | Mean | P-value1 | |
|---|---|---|---|
| Pre-test (N=9) | Post-test (N=9) | ||
| Minimum | 6.25 | 7.50 | 0.0199 |
| Median | 7.50 | 8.75 | |
| Mean | 7.50 | 9.03 | |
| Standard deviation | 0.62 | 1.04 | |
| Maximum | 8.75 | 10.00 | |
1 Wilcoxon Test. Level of significance alpha=5%
Source: prepared by the authors.
2-Satisfaction assessment
Nine participants completed the satisfaction questionnaire. The value calculated for Cronbach’s alpha coefficient was 0.793, with the consistency of this questionnaire being considered as “Acceptable”. The coefficient was calculated using the R programming language (R CORE TEAM, 2023)25.
Overall, the questionnaire responses were satisfactory for each of the items, with all of them ranging from “I Agree” to “I Fully Agree”, as shown in Graph 1.
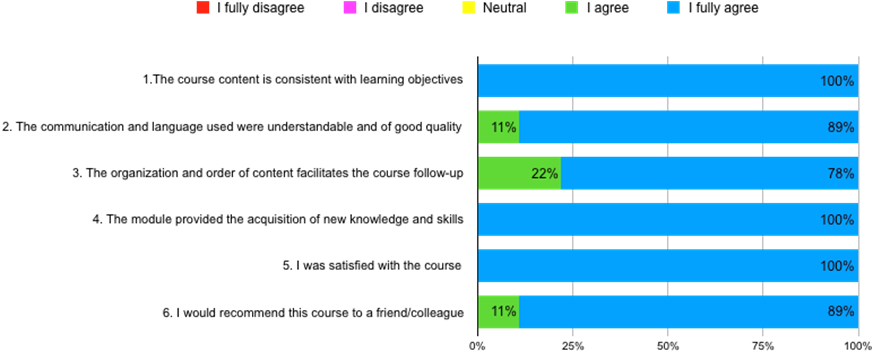
Source: prepared by the authors.
Graph 1 Assessment of student satisfaction with the teaching material “Patient Safety in the Anesthesiologist’s Practice”.
When asked if they would recommend other topics that they considered important for learning about PS in the anesthesiologist’s practice, and that were not covered by the teaching material, the participants answered “No” in their entirety, showing that they felt covered by the topics developed in the course. In the other open question, aimed at criticism, suggestions or praise for the teaching material presented, of the nine questionnaires answered, 4 participants answered:
“Excellent! Adequate time, well-selected questions. The question-based approach followed by theory is good for increasing engagement in the subject.”
“Approaches with questions lead to greater learning”
“It was great. Didactic and objective.”
“Congratulations, great material.”
Regarding the residents’ self-perception of the impact that the knowledge acquired through the teaching material could generate in relation to their practice, all answered favorably (Graph 2) with answers such as “I agree” and “I fully agree”.
DISCUSSION
The educational module “Patient safety in the anesthesiologist’s practice” was positively evaluated by 1st to 3rd-year anesthesiology residents, who considered its content relevant, with a potential positive impact on the residents’ training in the specialty on the specific topic, with high levels of satisfaction.
The methodology of assessing prior knowledge through pre-testing is recommended in the WHO Patient Safety Curriculum Guide26, which highlights the following benefits: establishing standards, the possibility of assessing the mastery of skills, prior knowledge and progress over time, establishing student classification, diagnosing the points of greatest difficulty, assessing the effectiveness of a course, and the possibility of providing feedback and motivation to students. Multiple-choice questions (MCQ) were considered by the Guide as appropriate formats for assessing student knowledge, but with the disadvantage that this assessment does not measure the applicability of knowledge in practice. Another point to be considered about MCQ is the testing effect. This effect refers to the idea that the test would not only have the function of assessing knowledge, but also improving the learning process27. Thus, the test effect also allows the use of MCQ as a teaching tool, with the ability to promote knowledge acquisition and retention for a longer period than other approaches, in a more adaptable manner28.
Although studies indicate low performance of residents regarding patient safety aspects due to the lack of more in-depth and effective knowledge, little appreciation of the topic and ineffective teaching5, the participants’ average pre-test scores (between 6.25 and 8.75, with an average of 7.5) was above 7.0, considered a positive finding. After the educational intervention, there was an increase in the average scores (9.03 - scores ranging from 7.5 to 10), with a significant difference to the values of the median grades, which demonstrates the effectiveness of the worked educational module on its objective of training anesthesiology residents on PS care.
Studies on strategies for the development and implementation of an educational module on PS aimed at anesthesiology residents and anesthesiologists are scarce4. Even with the understanding that education is a crucial factor for the continuous promotion of a safe environment, and that training in PS is the most important and most urgent task for a change in the safety culture,29 a curriculum on the subject, its approach and educational methods are not well established in the specialty. The available literature is mainly aimed at students in health areas or residents of various medical specialties.
In a study conducted with 120 students at the Johns Hopkins School of Medicine, a PS curriculum was developed and implemented and its impact on the medical students’ safety knowledge, self-efficacy and systemic thinking was evaluated30. Through the pre- and post-assessment of the students’ safety knowledge, self-efficacy in safety skills and systems-based thinking, in addition to the collection of satisfaction data, a significant improvement was observed in knowledge and systemic thinking scores, as well as a statistically significant increase in communication and safety skills taught and high satisfaction. The study highlights the need for further in-depth analysis of the long-term impact of this education on the students’ knowledge, skills, attitudes and behaviors30.
A randomized clinical trial6 evaluated the effectiveness of two types of online learning methodologies to improve PS behaviors required by the Joint Commission National Patient Safety Goals (NPSG) by 371 residents from different specialties. The study aimed to observe the impact on behavior, knowledge retention, and user satisfaction. Improvement in NPSG knowledge, NPSG-compatible behaviors in a simulation scenario, self-reported confidence in safety and quality, acceptability, and relevance of the program were evaluated. A simulation of central catheter insertion was included, and the goals defined for evaluation of the station were: improve communication effectiveness; improve patient identification accuracy; reduce the risk of healthcare-associated infection; comply with hand hygiene guidelines; perform pre-procedure verification process; and improve medication use safety.
The residents of that study who received the educational intervention completed an online satisfaction survey to assess their confidence and acceptability of the interventions on a Likert scale of 1 to 5, ranging from “I fully agree” to “I fully disagree”. The online learning programs improved knowledge retention and self-reported confidence. The study found a relatively poor performance for all trainees on the central line insertion simulation station and concludes that: there may be significant gaps in medical education in the PS area and that it is important to invest in educational programs in the area for young physicians. However, it considers the existence of multiple barriers to sustainable course integration, which included students, faculty and institutional factors6.
A study that systematically reviewed the quality improvement and patient safety curricula published for medical students and/or residents31 had the following objectives: to determine the applied educational content and teaching methodology; to evaluate the obtained learning outcomes; and to identify obstacles to curricular implementation. The content of the 41 evaluated curricula most frequently included topics such as continuous quality improvement, root cause analysis and systemic thinking. Regarding the methodology, the most commonly used design was the simple before-after comparison and courses with a workload that involved around 10 hours of contact and one to five meetings. Self-reporting was used as the method in the five studies that reported behavioral changes31. The curricula were generally well accepted, with significant improvements in knowledge acquisition in all studies. High satisfaction rates were obtained, usually assessed using a Likert scale, and one-third of the studies implemented changes in the provision of care31. A subsequent systematic review32 aimed to update this study and showed a similar conclusion.
The present study is compatible with data available in the literature on the implementation of a course on PS conducted with medical students and residents from different medical specialties, such as those presented previously. There are similarities between all these studies regarding several aspects. First, in relation to the choice of topics considered relevant, such as: general aspects of PS (key terminology and history), root cause/systems-based analysis, and the international goals established by the WHO and the Joint Commission International.
Second, regarding the adopted methodology, the design of the studies was the “before and after” type (pre- and post-intervention assessment of knowledge); assessment of satisfaction through post-intervention questionnaires on a Likert scale; assessment of perceptions of behavioral change through self-reporting and using personalized questionnaires with items corresponding to the learning objectives of the course.
Also, regarding the results obtained, there was good acceptance of the presented curricula, statistically significant improvements in the acquisition of knowledge and high satisfaction rates. Finally, some limitations were observed related to methodological issues, such as implementation in single centers and small samples; need to measure the long-term impact of interventions on students’ knowledge, skills, attitudes and behaviors; lack of evidence of the impact of educational interventions on patient outcomes.
In this sense, it was observed that the combination of the adopted pedagogical strategy associated with the protected time and space for the participation of residents in the present study were essential factors for the application of the educational module and for the positive results obtained. These findings highlight the importance of formally including the topic of PS in the curricular structure of residency courses, aiming to promote the acquisition of knowledge, attitudes and skills on the subject during the training process, in line with the recommendations of the WHO26 and the National Patient Safety Program1 of Brazil.
The available literature on the topic of education of anesthesiology residents in PS mainly deals with the importance of developing non-technical skills such as communication, leadership and teamwork, and the role of practical training in simulation as a fundamental tool33. However, most published studies make little reference to the theoretical basis applied, making it difficult to generalize results across different contexts34. According to expert consensus, the recommendation is that “investigators describe the theoretical basis for the chosen intervention components or provide an explicit logic model of why this patient safety practice should work” (34. Thus it is possible to better develop and select different approaches to PS education, evaluate their implementation, and allow generalizations.
Additional studies on patient safety education for anesthesiology residents are needed, especially regarding the ideal curriculum and its educational approach. Moreover, it is necessary to evaluate the extent to which educational interventions influence change in behavior or skill development in residents, whether these changes are sustained, and whether they are capable of bringing practical results to patients. However, such research is inherently challenging, since, due to the size of residency programs, sample sizes are often small and student randomization may be unethical or impractical35. Furthermore, studies using methodologies that allow the assessment of parameters at higher levels of the Miller pyramid, such as the application of knowledge acquired by residents, problem-solving, and positive impact on patients, may be difficult and require institutional support.
The practice of anesthesiology involves manual skills and management in a complex system. Thus, the development and implementation of educational approaches in PS for this group requires evidence-based practices to improve the most diverse skills. The teaching and assessment of these skills require active learning methodologies, such as through simulation and structured clinical examinations, as well as resident participation in the analysis of adverse events and involvement in improvement projects related to patient safety4.
CONCLUSION
The educational strategy developed and applied in this study proved to be effective for the training of anesthesiology resident physicians on the topic of patient safety, as the acquisition of knowledge and the high levels of acceptance and satisfaction were increased. In this sense, a difference was observed when protected time and space were offered for the acquisition of knowledge, attitudes and skills on the topic during the training process, inferring that the formal inclusion of the topic of patient safety in the curricular structure of residency courses is a path with great potential for success.
However, further studies are needed to measure the long-term impact of this strategy, its influence on the acquisition of skills and whether it results in better outcomes for patients.
REFERENCES
1. Brasil. Portaria nº 529, de 1º de abril de 2013. Institui a Política Nacional de Segurança do Paciente (PNSP). Diário Oficial da União; 2013 [acesso em 20 fev 2024]. Disponível em: Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/gm/2013/prt0529_01_04_2013.html . [ Links ]
2. Mellin-Olsen J, Staender S, Whitaker DK, Smith AF. The Helsinki Declaration on patient safety in anaesthesiology. Eur J Anaesthesiol. 2010;27(7):592-7. [ Links ]
3. Brasil. Resolução n° 11, de 8 de abril de 2019. Dispõe sobre a matriz de competências dos Programas de Residência Médica em Anestesiologia no Brasil. . Diário Oficial da União ; 2019 [acesso em 9 jan 2024]. Disponível em: Disponível em: http://portal.mec.gov.br/index.php?option=com_docman&view=download&alias=111551-11-resolucao-n-11-de-8-de-abril-de-2019-anestesiologia&category_slug=abril-2019-pdf&Itemid=30192 . [ Links ]
4. Harbell M, Methangkool E. Patient safety education in anesthesia: current state and future directions. Curr Opin Anaesthesiol. 2021;34:720-5. [ Links ]
5. Pereira FSH, Garcia DB, Ribeiro ER. Identifying patient safety competences among anesthesiology residents: systematic review. Braz J Anesthesiol. 2022;72(5):657-65. [ Links ]
6. Shaw TJ, Pernar LI, Peyre SE, Helfrick JF, Vogelgesang KR, Graydon-Baker E, et al. Impact of online education on intern behaviour around joint commission national patient safety goals: a randomised trial. BMJ Qual Saf. 2012 Oct;21(10):819-25. [ Links ]
7. Sousa VD, Driessnack M, Mendes IAC. Revisão dos desenhos de pesquisa relevantes para enfermagem: Parte 1: desenhos de pesquisa quantitativa. Rev Lat Am Enfermagem. 2007;15(3):502-7. [ Links ]
8. Zambon LS, Daud-Gallotti R, Novaes HMD. Introdução à segurança do paciente. Proqualis; 2010 [acesso em 5 set 2023]. Disponível em: Disponível em: https://proqualis.fiocruz.br/aula/introdu%C3%A7%C3%A3o-%C3%A0-seguran%C3%A7a-do-paciente . [ Links ]
9. Organização Mundial da Saúde. Segundo desafio global para a segurança do paciente. Cirurgias seguras salvam vidas. Rio de Janeiro: Organização Pan-Americana da Saúde; 2009. [ Links ]
10. Cangiani LM, Carmona MJC, Torres MLA, Bastos CO, Ferez D, Silva ED, et al., editores. Tratado de anestesiologia da Sociedade de Anestesiologia do Estado de São Paulo. 8a ed. São Paulo: Atheneu; 2017. [ Links ]
11. Agência Nacional de Vigilância Sanitária. Assistência segura: uma reflexão teórica aplicada à prática. 2a ed. Brasília: Anvisa; 2017. [ Links ]
12. World Health Organization. Global patient safety challenge: 2005-2006. Geneva: WHO; 2005. [ Links ]
13. Agência Nacional de Vigilância Sanitária, Organização Pan-Americana da Saúde. Manual para observadores: estratégia multimodal da OMS para a melhoria da higienização das mãos. Desafio: uma assistência limpa é uma assistência mais segura. Aliança Mundial para Segurança do Paciente. Brasília: Organização Mundial da Saúde; 2008. [ Links ]
14. Medication Without Harm. Global patient safety challenge on medication safety. Geneva: World Health Organization; 2017. [ Links ]
15. Agência Nacional de Vigilância Sanitária. Protocolo de segurança na prescrição, uso e administração de medicamentos. Brasília: Ministério da Saúde; 2013 [acesso em 5 set 2023]. Disponível em: Disponível em: https://www.gov.br/anvisa/ptbr/centraisdeconteudo/publicacoes/servicosdesaude/publicacoes/protocolo-de-seguranca-na-prescricao-uso-e-administracao-de-medicamentos/view . [ Links ]
16. Metzner J, Posner KL, Lam MS, Domino KB. Closed claims’ analysis. Best Pract Res Clin Anaesthesiol. 2011;25(2):263-76. [ Links ]
17. Posner KL. Closed claims project shows evolution. Anesthesia Patient Safety Foundation; 2001 [acesso em 10 jan 2024]. Disponível em: Disponível em: https://www.apsf.org/article/closed-claims-project-shows-safety-evolution/ . [ Links ]
18. Moura GHS, Dias RX. Eventos adversos em anestesia. Anestesia em Revista. 2016; 3:18-9. [ Links ]
19. Lemos Neto SV de, Diego LAS, Brandão JCM, Silva JH, Carneiro AF, editores. Segurança do paciente e prática médica. Rio de Janeiro: Sociedade Brasileira de Anestesiologia; 2014. [ Links ]
20. Cook TM, Woodall N, Frerk C. Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: Anaesthesia. BJA Open. 2011 May;106(5):617-31. [ Links ]
21. Apfelbaum JL, Hagberg CA, Connis RT, Abdelmalak BB, Agarkar M, Dutton RP, et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022;136(1):31-81. [ Links ]
22. Cassorla L, Lee JW. Patient positioning and associated risks. In: Miller RD. Miller’s anesthesia. 8th ed. Philadelphia: Elsevier, Saunders; 2015. p. 2594-639. [ Links ]
23. Salman FC, Diego LAS, Silva JH, Moraes JMS de, Carneiro AF, editores. Qualidade e segurança em anestesiologia. Rio de Janeiro: Sociedade Brasileira de Anestesiologia; 2012. [ Links ]
24. Agência Nacional de Vigilância Sanitária; Organização Pan-Americana da Saúde. Mecanismos para a prevenção de quedas dos pacientes - protocolos de segurança do paciente II. Brasília: Anvisa , Opas; 2018. [ Links ]
25. R CORE Team. R: a language and environment for statistical computing. Version 4.3.2. Vienna: R Foundation for Statiscal Computing; 2023. [ Links ]
26. Organização Mundial da Saúde. Guia curricular de segurança do paciente da Organização Mundial da Saúde: edição multiprofissional. Rio de Janeiro: Autografia; 2016. 270 p. [acesso em 23 fev 2024]. Disponível em:Disponível em:http://apps.who.int/iris/bitstream/handle/10665/44641/9788555268502-por.pdf?sequence=32 . [ Links ]
27. Panúncio-Pinto MP, Troncon LE de A. Avaliação do estudante - aspectos gerais. Medicina (Ribeirão Preto). 2014;47(3):314-23 [acesso em 23 fev 2024]. Disponível em: Disponível em: https://www.revistas.usp.br/rmrp/article/view/86684 . [ Links ]
28. Bezerra MG, Silva ME de S, Silva CM e, Costa MLWFG, Borges JM, Spirandelli APB, et al. Efeito teste e sua real eficácia na aprendizagem e retenção de conhecimento. Braz J Hea Rev. 2023;6(5):22142-51. [ Links ]
29. Rall M, van Gessel E, Staender S. Education, teaching & training in patient safety. Best Pract Res Clin Anaesthesiol. 2011;25(2):251-62. [ Links ]
30. Aboumatar HJ, Thompson D, Wu A, Dawson P, Colbert J, Marsteller J, et al. Development and evaluation of a 3-day patient safety curriculum to advance knowledge, self-efficacy and system thinking among medical students. BMJ Qual Saf . 2012;21:416-22. [ Links ]
31. Wong BM, Etchells EE, Edward E, Kuper A, Levinson W, Shojania KG. Teaching quality improvement and patient safety to trainees: a systematic review. Acad Med. 2010;85(9):1425-39. [ Links ]
32. Kirkman MA, Sevdalis N, Arora S, Baker P, Vincent C, Ahmed M. The outcomes of recent patient safety education interventions for trainee physicians and medical students: a systematic review. BMJ Open. 2015;5(5):e007705. [ Links ]
33. Garcia DB. Avaliação do conhecimento de residentes do terceiro ano em anestesiologia sobre a segurança do paciente [dissertação]. Curitiba: Faculdade Pequeno Príncipe; 2021. [ Links ]
34. Foy R, Ovretveit J, Shekelle PG, Pronovost PJ, Taylor SL, Dy S, et al. The role of theory in research to develop and evaluate the implementation of patient safety practices. BMJ Qual Saf . 2011 Feb 11;20(5):453-9. [ Links ]
35. Martinelli SM, Isaak RS, Schell RM, Mitchell JD, McEvoy MD, Chen F. Learners and luddites in the twenty-first century: bringing evidence-based education to anesthesiology. Anesthesiology. 2019;131:908-28. [ Links ]
Received: March 07, 2024; Accepted: August 13, 2024











 texto em
texto em