Serviços Personalizados
Journal
Artigo
Compartilhar
Revista Brasileira de Educação Especial
versão impressa ISSN 1413-6538versão On-line ISSN 1980-5470
Rev. bras. educ. espec. vol.26 no.1 Marília jan./mar. 2020 Epub 12-Fev-2020
https://doi.org/10.1590/s1413-65382620000100003
Research Report
Effects of the Use of Assistive Technology Devices to Promote Independence in Daily Life Activities for a Child with Cerebral Palsy2
3Undergraduate in Occupational Therapy. Federal University of São Carlos. São Carlos/São Paulo/Brazil. Email: thaisbretzlino@gmail.com.
4Occupational Therapist. PhD in Bioengineering. Professor of the Occupational Therapy Department at Federal University of São Carlos. São Carlos/São Paulo/Brazil. Email: luagnelli@ufscar.br.
5Psychologist. Doctor in Special Education. Professor at the Department of Education and the Graduate Program in Education at the Federal University of Paraná. Curitiba/Paraná/Brazil. Email: boueri.iasmin@gmail.com.
6Occupational Therapist. Doctor in Special Education. Professor at the Occupational Therapy Department and the Special Education Graduate Program at Federal University of São Carlos. São Carlos/São Paulo/Brazil. Email: gerusalourenco@gmail.com.
The objective of this study was to evaluate the implementation process of Assistive Technology resources to perform the feeding activity of a child with cerebral palsy. A five-year-old child with dystonic cerebral palsy and his mother were the participants. The target activities were feeding and intervention that occurred at their home. Data were collected by the following instruments: Pediatric Evaluation of Disability Inventory; Gross Motor Function Classification System for Cerebral Palsy; Manual Abilities Classification System; script to characterize the participant; descriptive and event logging protocols; and a social validation questionnaire. Interventions were performed with three activities for feeding independence: sitting at the table, using the glass and the cutlery. The activities comprised the multiple baseline design between behaviors in four phases: baseline, intervention, maintenance and follow up. The sessions were recorded on video for analysis and help level scoring in the event protocol. Score of the help level in the protocol of events. It was evidenced that the use of Assistive Technology resources enhances the autonomy and independence of the child with cerebral palsy, demonstrating the effectiveness of the use of the resource, corroborating the literature.
KEYWORDS: Special Education; Assistive Technology; Cerebral Palsy; Occupational Therapy
O objetivo deste estudo foi avaliar o processo de implementação de recursos de Tecnologia Assistiva para realização da atividade de alimentação junto a uma criança com paralisia cerebral. Foram participantes uma criança de cinco anos com paralisia cerebral distônica e sua mãe. As atividades-alvo foram a alimentação e a intervenção que ocorreram em seu domicílio. Os dados foram coletados pelos seguintes instrumentos: Inventário de Avaliação Pediátrica de Incapacidade; Sistema de Classificação da Função Motora Grossa Ampliado e Revisto; Sistema de Classificação de Habilidade Manual para Crianças com Paralisia Cerebral; roteiro para caracterização do participante; protocolos de registro descritivo e de eventos; e questionário de validação social. Foram realizadas intervenções com três atividades para independência na alimentação: senta-se à mesa, uso do copo e uso do talher. As atividades compuseram o delineamento de linha de base múltipla entre comportamentos em quatro fases: linha de base, intervenção, manutenção e follow up. As sessões foram registradas em vídeo para análise e pontuação do nível de ajuda no protocolo de eventos. Evidenciou-se que o uso de recursos de Tecnologia Assistiva potencializa a autonomia e independência da criança com paralisia cerebral, demonstrando a efetividade do uso do recurso, corroborando com a literatura.
PALAVRAS-CHAVE: Educação Especial; Tecnologia Assistiva; Paralisia Cerebral; Terapia Ocupacional
1 Introduction
Cerebral palsy is characterized by non-progressive neuropathological disorders that occur in children up to two years old, encompassing a series of different clinical syndromes, which may or may not be associated with cognitive impairment (Brandão, Oliveira, & Mancini, 2014; Monteiro, Vasconcelos, Silva, & Calvacante, 2012; Silva & Pontes, 2016).
Depending on the area of the affected nervous system, the individual is affected in different ways, presenting disorders marked by the lack of control over movements that can impair functional performance (Brandão, Oliveira, & Mancini, 2014; Mancini et al., 2004; Pfeifer et al., 2014; Silva & Araujo, 2019; Sposito & Riberto, 2010). Studies indicate that most children with cerebral palsy have some kind of motor disorder that directly impacts their daily lives, influencing their way of controlling their environment, independence and autonomy (Guerzoni et al., 2008; Martins, Müller, & Heidrich, 2008; Ostensjo, Carlberg, & Vollestad, 2005). Thus, most of these children require an extensive assistance to perform day-to-day activities such as self-care (Ostensjo, Carlberg, & Vollestad, 2005).
Literature indicates that Assistive Technology (AT) can help them to gain independence and control of the environment, favoring its exploration, control of space and experience in their multiple life contexts (Copley & Ziviani, 2004; Cowan & Khan, 2005; Earde, Praipruk, Rodprait, & Seanjumla, 2018; Ostensjo, Carlberg, & Vollestad, 2005; Watson, Ito, Smith, & Anderson, 2010).
AT is an area of knowledge that consists of assisting persons with disabilities in the performance of their duties, not being limited only to the resources offered, but also covering the direct assistance available, selection, acquisition and/or training of a device. Its concept is broad, and resource development has allowed the appreciation, integration and inclusion of many people, promoting their human rights and their participation (Cook & Polgar, 2015; Cowan & Khan, 2005).
The resources of AT are organized in modalities and their classification may vary according to the different authors or institutions that work with it, such as equipment for self-care activities, mobility and communication, among others. The characteristics of AT recommendations are driven by the needs, objectives, capabilities, skills and desired roles of the consumer and should be considered in assessing his/her purposes, interests and desire, as well as those of his/her family, caregivers, and the context in which this individual is inserted (Cook & Polgar, 2015; Trombly & Radomski, 2005).
The AT implementation process is integrated and should involve the performance of a multidisciplinary rehabilitation team, with different stages, namely: the assessment of the patient and of the existing and used devices; the assessment of the demands of the patient, his/ her family and caregiver; the prescription of an AT resource and its preparation; training to use it with a patient, teachers, caregivers and/or family members; monitoring the use and periodic reevaluations that may cause adaptations, modifications or replacement of resources; and possible locations for the use of the resource (Cook & Polgar, 2015; Cowan & Khan, 2005; Fachinetti, Gonçalves, & Lourenço, 2017; Sposito & Riberto, 2010; Trombly & Radomski, 2005).
Studies by Ostensjo, Carlberg and Vollestad (2005) and Cowan and Khan (2005) describe the impact of AT devices on daily life activities and the care of children with cerebral palsy as beneficial, pointing out the effectiveness of their use when inserted in the early life of these children and demonstrating the importance of prescription and use of AT in childhood. However, it lacks studies that describe the step-by-step implementation of AT resources, such as decision making and operationalization of resource-making steps for children with cerebral palsy in the context of daily living activities, which would assist in the reasoning of the professionals involved at the time of prescription. Reliable scientific evidence would favor the appropriate indication of resources that enable the social participation and autonomy of people with disabilities, but little is found in the literature on the impacts of their use on daily life and on the promotion of functionality in daily activities through substantiated evidence (Copley & Ziviani, 2004; Cury & Brandão, 2011).
Thus, the hypotheses posed in the study were: it is possible to prescribe AT resources that favor feeding activity with a child with cerebral palsy through a home intervention focused on the demands of family routine; the decision-making process for the most appropriate equipment can be made through the child’s functional performance during the activity, with the systematization of continuous data throughout the intervention. In this sense, the aim of the study was to investigate and evaluate the process of implementing AT resources for feeding activity with a child with cerebral palsy.
2 Methodology
This paper is characterized as experimental research on a single subject design. In this study model applied to the participant’s reality, it is sought to control the dependent, independent and intervening variables (Gast & Ledford, 2014). There is the independent variable, characterized by the assistive technology resources, which is programmatically inserted at different times and its effect is observed in the dependent variable, behaviors performed in the selected feeding activities. The intervening variables were observed and reported in order to enable better intervention schedules for future studies. The use of this design allows the researcher to plan when interventions will be implemented and to observe their effects. The multiple baseline design between behaviors, being a single subject derivative (Gast & Ledford, 2014), was chosen for this research in order to allow the inference of program effects.
2.1 Ethical procedures
The project was approved by the Human Research Ethics Committee with Opinion no. 761.522, CAAE: 33534614.1.0000.5504, and all procedures performed respected the principles of the National Health Council regarding the Guidelines and Regulatory Norms for Research involving Human Beings.
2.2 Research location
The research was conducted at the participant’s house, where the child and his/her parents reside. The sessions took place in the outdoor area of the house, containing a table with four armless plastic chairs and a plastic armchair. When it rained, the session was held in the kitchen.
2.3 Participants
The participants were a 5-year-old boy diagnosed with Dyskinetic Cerebral Palsy (Dystonic) grade III on the Gross Motor Function Classification System for Cerebral Palsy (GMFCS) and the Manual Ability Classification System for Children with Cerebral Palsy (MACS), and his mother. The participant presents abnormal postures and involuntary and intermittent muscle contractions. The dystonia presented by him is exacerbated during the intentional movements of the limbs, consequently interfering in the functional performance in daily activities, including those analyzed by this study. Although the predominant clinical feature is dystonia, the child has increased muscle tone in all four limbs.
Due to neurological changes, there is impairment of global motor coordination and, especially, fine motor coordination, with difficulty in decoupling the distal movements of the upper limbs and to perform precise movements such as reaching and grasping objects. He therefore benefits from resources that aid in postural stability and adaptations for attaching or stabilizing utensils, such as grip-replacement accessories. Due to the high tone, he uses positioning orthoses for the upper and lower limbs, as well as functional orthoses for thumb abduction.
The self-care scale of the Pediatric Evaluation of Disability Inventory (PEDI) instrument indicated a gross score of 28 and a normative score below 10 without standard error. The continuous score presented was 47.82 and standard error of 2.16. In part II, about caregiver assistance, the child obtained 3, presenting a normative score below 10, with no standard error. The continuous score was 29.82, with a standard error of 7.60. And in part III, the mother pointed as no modification (eight items) in the area of self-care. Thus, it was identified the independent feeding difficulty of the child, having indication for the implementation of AT resources.
2.4 Participant characterization instruments
The instruments used were:
Participant characterization script.
Extended and Revised Gross Motor Function Classification System (GMFCS E & R) (Hiratuka, Matsukura, & Pheifer, 2010; Silva, Pheifer, & Funayama, 2010a).
Manual Ability Classification System for children with cerebral palsy 4-18 years - MACS (Silva, Pheifer, & Funayama, 2010b).
2.5 Instruments for data collection
The instruments used were:
Pediatric Evaluation of Disability Inventory - PEDI (Mancini, 2005): in order to characterize the child’s performance at the beginning and end of the intervention.
Protocol for Descriptive Registration: used to record situational observations that occurred during clinical care sessions, allowing to observe the input behavioral repertoire regarding the use of Assistive Technology resources.
Event Registration Protocol: elaborated from the analysis and observations of the activities to be performed and aimed to verify if there was a change in the participant’s behaviors from the implementation of AT resources and to record the levels of help used to perform the task with the implementation of the AT resource, on an ordinal scale ranging from score 5 (five), if the child performed the task independently, without any help or assistance; to score 0 (zero) if the child did not perform the task. Intermediate scores describe the varying amount of help provided to children, such as verbal hint (score 4), demonstrative hint (score 3), partial physical help (score 2) or total physical help (score 1).
Social Validation Questionnaire: it aimed to record the mother’s statements and considerations regarding the entire process that involved the research through eight questions.
2.6 Intervention
An intervention program was elaborated based on the baseline data, in which the main researcher became aware of the participant’s initial repertoire in performing the feeding activities. To implement the proposed program, three activities that make up the diet were selected: sitting at the table, using the glass and using the cutlery. Decision making for the implementation of resources was based on the child’s pace and responses, not being able to predict all stages of the intervention program, but adjusting to each session according to the child’s needs and demands (Cook & Polgar, 2015). Chart 1 presents the description of the skills involved in each activity worked with the child.
Table 1 Presentation of the basic skills contained in the assessment protocol.
| SITTING AT THE TABLE | |
| Sit at the table Torso control Positioned feet Arms positioned Approach the table Pull chair near table Reach table objects Pull chair near table |
Go to the table and be positioned in the chair next to the table. Keep torso erect and move it for posture adjustment. Feet flat on the floor or footrest. Hands resting on the armrest, table or side of the chair close to the torso. Lean the body close to the table. Grasp the chair and pull it close to the table. Take an object on the table, using the hand or fingers. Grasp the chair and pull it close to the table. |
| USE OF THE GLASS | |
| Hold glass with the liquid in it. Lean the glass towards the mouth Get the glass Glass drinking position Position the straw Head direction to the glass Drink the liquid Back to the starting position |
Keep the glass in hand with the liquid inside. Perform pronation of the forearm, with shoulder flexion bringing the glass to the mouth. Hold the glass with the hand. Drag the glass and set it close to the body in order to drink, with the use of the arm and/or hand. Straighten the straw with the hand, turning it towards the mouth. Lean the torso and straighten the head towards the glass and/or the straw to drink. Drink/swallow the liquid from the glass. With the arm and/or hand push the glass, returning it to the starting position. |
| USE OF THE CUTLERY | |
| Pick up the cutlery Handle the cutlery Add the food Cut the food Put the food on the cutlery (or jab it) Bring food to mouth Return with the fork towards the table. |
Reach the cutlery with the hand. Hold the cutlery with the hand. Put a quantity of food together, with the cutlery. Cut a piece of food into pieces, with the use of a knife. Push the food with the knife and place it on the fork. Bring the fork with food to the mouth. Return of the fork to the table. |
Source: Elaborated by the authors based on Windholz (2016).
The process of intervention of the activities involved the following actions with the child:
Activity 1 - “Sitting at the Table”: All the tables and chairs in the house were tested to seewhich offered proper placement. A chair and table that would allow more stability for the child were chosen and a footrest was proposed, initially presented to the child and explained how it would be used. To adapt the seat and the backrest of the chair, different foam types were tested to better support the child. After the size and thickness of the foam had been adjusted, they were sent to an upholsterer, who lined them with sturdy and hygienic fabric. With these resources, the child showed stability in his independence level before the implementation of activity 2.
Activity 2 - “use of the glass”: several types of cups were tried in order to test which one would allow more autonomy on the part of the child, namely: single-handle cup and spout, one plastic handle cup and one other of elastic, cut-out glass, tall glass with plastic straw, glasses with different heights, different straws. Due to the child’s motor difficulties resulting from spasticity and limitation of active range of motion in the upper limbs, the use of a cup with lid and straw was implemented so that the child did not have to hold and/or move the glass up to his mouth in order to drink.
Activity 3 - “use of cutlery”: much of the child’s movements in this activity depended on the researcher’s help. The spoon had to be placed in the child’s hand and the upper limb moved with assistance (to place the food on the spoon and move it towards the mouth). Spoons with angled handles, with EVA and foam thickeners, spoon with handle made of plastic, and a conventional fork and spoon were tested. The child was prescribed a Neoprene orthosis for both hands; and in sessions he had this resource, a functional gain was verified in his grip. However, the child refused to use this device, despite the researcher’s encouragement. This refusal was also reported by the mother in other daily activities.
2.7 Assessment of assistant technology resource implementation
The program was applied for six months and the sessions varied in duration (from 20 minutes to an hour and a half), depending on the activity being performed. Four experimental phases were performed that composed the multiple baseline design between behaviors:
Baseline: observation and recording of the participant’s feeding activity with his caregiver.
Intervention: implementation of the Assistive Technology resource, guidance to family members and activity training.
Maintenance: In order to verify that the change that occurred after the intervention period and the implementation of the Assistive Technology resource remained without continuous intervention.
Follow up: occurred three weeks after completion of the intervention and maintenance phases with the participant, for a reassessment of the continuity of gains and behaviors acquired.
The change for each of the phases was conditioned to behavioral stability with the criterion of obtaining 60% or more independence in performing the activity using the resource in at least three consecutive sessions, except for activity 3. In this activity the criterion adopted to start maintenance was another, since it would not be possible to achieve 60% independence in a short period. As the child’s response stabilized during three consecutive sessions with the mother’s help, it was decided to move to the maintenance phase in order to complete the study.
2.8 Data collection procedures
After the ethical procedures and the selection of the research participants, the PEDI, MACS and GMFCS instruments were applied with the mother towards the characterization of the child. Subsequently, we began collecting data from the behavioral multiple baseline design, which consisted of filming and using the event log protocol during all experimental phases of the study (baseline, intervention, maintenance, and follow-up). During all sessions, the field diary script was completed and events were recorded. These records were supported by the filming of the sessions with the participant and made it possible to follow the participants’ involvement, suggestions, considerations and difficulties faced during the implementation process of the proposed intervention. Finally, the PEDI instrument was reapplied as a measure of the child’s performance in his natural context six months after the first assessment, and the social validation questionnaire was applied to the child’s mother.
2.9 Data analysis procedures
For the analysis of the proposed intervention, a multiple behavioral baseline design was applied (Gast & Leadford, 2014), with the child’s performance systematization recorded at each proposed phase during the AT resource implementation procedures. The data supported decision making on changes in the resources prescribed in each activity by the occupational therapist.
2.10 Interobservers concordance
Reliability tests were performed during the study on 25% of the observations of each experimental phase. For this, the sessions were recorded and the videos were presented to the researcher’s assistant (a student of the last semester of the Occupational Therapy undergraduate course). When attending the sessions, the assistant was instructed to fill out the registration protocol, guiding the operationalizations and descriptions of behaviors and taking into consideration an ordinal scale that ranged from score 5 (five) to score 0 (zero). The protocols completed by the researcher and the research assistant were analyzed point by point and the interobserver concordance index was calculated, concordance percentage is equal to the total concordance divided by the sum of the concordance and discordance points (Gast & Ledford, 2014). After performing the calculation, the concordance range was greater than 75% between the records of the principal researcher and the research assistant.
3 Results
The results were obtained by applying the event protocol on the participant’s independence level and the level of assistance offered for teaching during all experimental phases of the study and in all proposed activities. The proposition of changes in seat heights in activity 1; in the types of glasses and straws, in activity 2; and cutlery, in activity 3, could occur based on the performance that the child obtained in the session.
In Figure 1, the abscissa axis shows the participant’s independence percentage, ranging from 0 to 100%; the ordinate axis marks the day of the session in which the participant reached the represented percentage. In gray columns are the assistance levels obtained per session. The dotted line divides the sessions into the phases in which they were made.
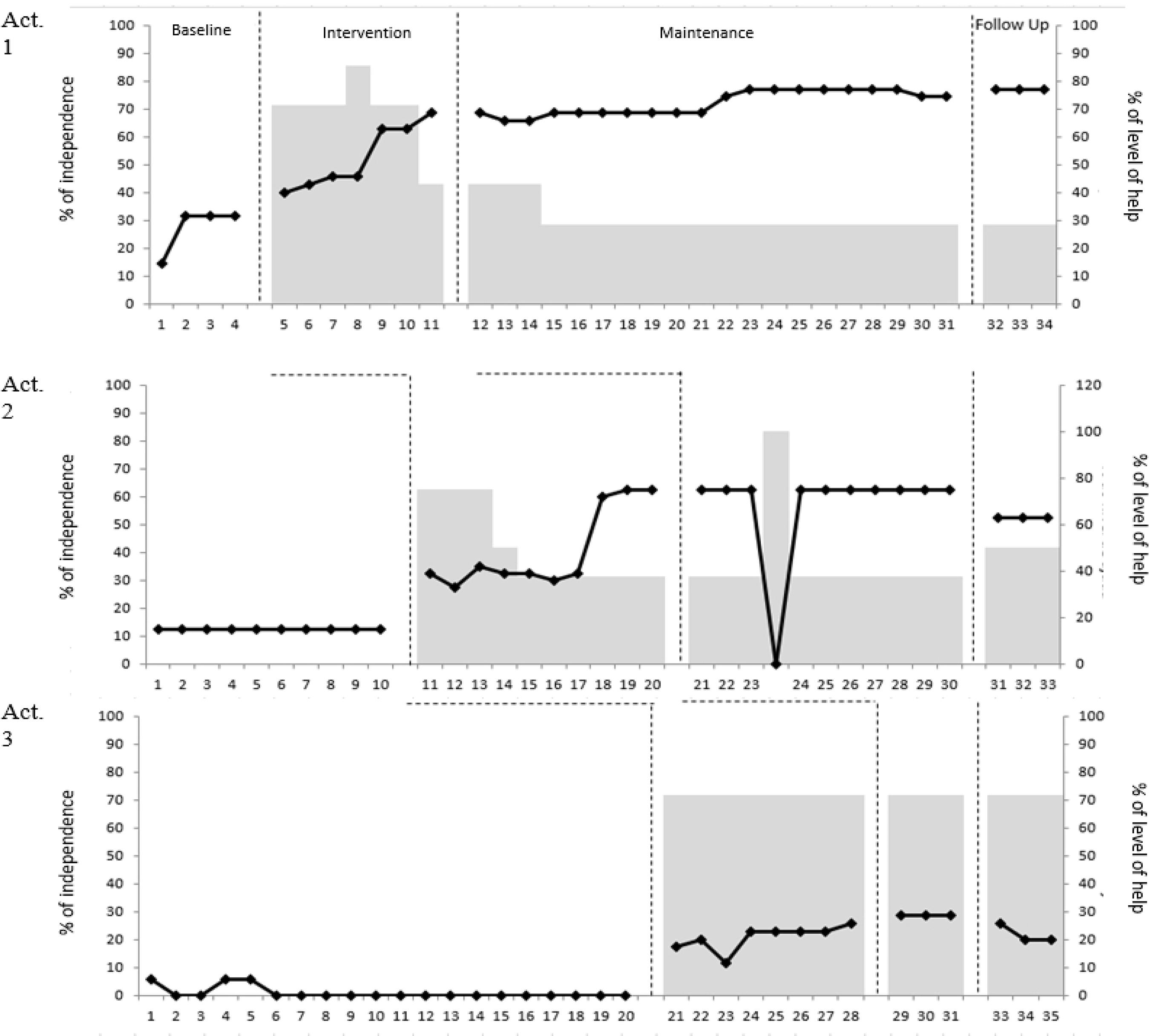
Source: Elaborated by the authors.
Figure 1 Percentage of participant independence to perform the activity (black line) and levels of assistance provided by the researcher (gray columns).Legend: Act. - Activities taught.
When verifying the data obtained during the baseline, in activity 1, which consisted of sitting at the table, the child presented a percentage of independence for the activity performance of 14 to 31%, presenting an average of 26,75% independence to accomplish it. With the beginning of the intervention, the change in the percentage of independence was observed, with an abrupt increase. It can be seen that the percentage of independence begins to increase, reaching a 69% independence at the end of the seven practice sessions. After the intervention was completed, this activity began to be maintained and, from the 22nd session, the child began to show an increase in independence, reaching 77% of independence. In the follow up phase, the child had 77% independence during three sessions. In this activity, no behavior was performed independently in the baseline phase, with most of the task being considered as dependent. In the intervention sessions, it was possible to gradually observe the decrease in the dependency level and the increase of partial assistance. Assistance levels varied during sessions, for example, in session 9, 10 and 11 it is possible to verify the presence of verbal hint. In the maintenance phase, total physical assistance stabilized at 30%, obtaining variations in partial assistance, verbal hint and demonstrative hint. In the follow-up phase, assistance levels stabilized, with a score of 30% total assistance and 70% independence.
In activity 2, in which the child learned to use the glass, the data obtained during the baseline presented a constant independence percentage of 13%. When the interventions started, after activity 1, he had reached the 60% independence criterion, it was clearly observed the participant’s increased independence in performing the activity, which reached 63% in the last two sessions prior to the maintenance phase. During the maintenance phase, the child maintained his level of independence in this activity, in the 24th session, in which he zeroed, not because of inability to perform the activity, but because the child did not have the opportunity to do this activity that day. During follow up, the child maintained 53% independence.
As for the levels of assistance, at baseline, the child depended on help 95% of the time, and had only 5% independence in carrying out the activity. In the intervention phase, assistance levels varied as the various AT strategies and resources were implemented and the level of independence increased. In the maintenance phase, the level of dependence stabilized at 40%, achieving 60% independence in this activity. Except for session 26, in which the child presented 100% dependence, being the session in which the child had no opportunity to perform the task, since he did not use the glass that day. At the follow-up, the child maintained the dependence level at 40%, with 10% total physical assistance and 50% independence. According to the mother’s report, the speech therapist who accompanied the child observed changes and improvements in his swallowing due to the use of the drinking glass offered to the child. The child became increasingly independent, adjusting the limitations for his use.
In activity 3, the use of cutlery during the baseline phase, the child showed total dependence to perform the activity, scoring 0% independence. After activity 2 reached the 60% independence criterion, the implementation of AT resources for the third activity was started. At the beginning of the intervention phase, he presented a performance percentage of 17 to 26% independence, reaching an average of 20.75% independence. During the maintenance phase reached 26% independence, achieving the same score in the three consecutive sessions. At the follow up, the performance was 20 to 26% independence. Thus, at baseline, almost 100% dependence was identified in the activity, except for sessions 1, 4 and 5, which presented 30% of total physical assistance and 70% of dependence, as he actively sought to use the cutlery.
In the intervention phase, the level of total physical assistance increased, varying with dependence and partial physical assistance. In this activity of using the cutlery, the child was very resistant to follow the researcher’s guidelines and to accept her assistance, even when the amount of food was negotiated. In some encounters, the child refused to eat and cried too much. Due to physical limitations and difficulties in dealing with the child who refused to eat, the mother took part in the activity, which helped the child to use the resources. She was instructed on how to stand behind the child, where to hold and how to perform the movement with the child. In the maintenance phase, the total assistance level remained at 60% and 40% partial assistance. During follow up, the child increased the level of total physical assistance.
Regarding the reapplication of the PEDI instrument after 6 months in the self-care functional skills, the gross score obtained was 32, with a normative score below 10, without standard error, with a continuous score of 50.80 and a standard error of 2.09. Regarding caregiver assistance in the self-care area, the gross score obtained was 12, with a normative score below 10 without standard error. The continuous score was 53.38 and its standard error 4.26.
Changes in gross and continuous scores could be observed, which may indicate a gain in ability, but in relation to the normative score, the child still scores below 10. Despite the increase, the change does not reach the predicted results that would be considered as a clinically significant difference for the instrument (Iyer, Haley, Watkins, & Dumas, 2003). However, in Part III of the instrument, which identifies the number of functional activities for which modifications are required, it was possible to visualize changes with the proposed intervention. The first time the test was applied, it was pointed out that the eight items presented by the instrument needed changes, and in the reevaluation, there were seven, since in the food item, the presence of child-centered modification was identified as the resources that were implemented in the research.
Finally, regarding the results related to social validity, the mother reported, in general, that the child presented improvements and evolution, increasing the level of autonomy and independence in feeding. From 0 to 5, she gave the research a score of 3 because, according to her, she had expectations that her child would obtain total autonomy in the feeding activity. The mother also pointed out how much the research helped her to allow her child’s development and to be more patient with the learning process, respecting his time and limitations. She considered that the research had impacted on her family routine, by changing the family dynamics, now sitting at the table to eat along with the child and by arousing the child’s interest in eating more independently, expanding his attempts in other spaces, such as school and restaurants.
4 Discussion
The data obtained by the study indicate that the use of the proposed AT resources impacted the child’s feeding activities, allowing an enhancement towards his autonomy, even occurring in a short time frame for such an intervention. This reinforces the relevance of the use of AT in the interventions of children with cerebral palsy mentioned by Cowan and Khan (2005) and Ostensjo, Carlberg and Vollestad (2005), with beneficial impacts and effectiveness of these resources in their daily lives, in order to offset the functional demands for their independence and directly impacting the performance of ADLs, by reducing the amount of aid required for performance of the activity.
Cury and Brandão (2011) and Novak, Smithers-Sheedy and Morgan (2012) argue that the goal of intervention with a child with Cerebral Palsy is to increase his/her functional independence, promoting his/her abilities, mobility, cognitive development and social interaction. Due to his/her limitations, the child cannot complete the daily activities; thus, the authors point out that the use of AT resources is to increase, maintain and promote function and independence.
For the implementation process, after evaluating the child’s functional skills and observing the research entry repertoire, it was possible to identify the stages of the activities that needed modifications to enable an autonomy and independence gain, in order to think about which resources and strategies would be taken to achieve the proposed goals. Each step represents the implementation process, addressing the procedure for inserting resource use, training, reevaluation, readjustment or replacement of the resource until the proposed objectives are achieved.
We chose to teach each activity gradually, inserting the resources progressively and their use through the child’s response, obtaining the presence of participant-centered modifications. Thus, each decision was taken along the process of prescription and use of resources based on the behavioral responses issued by the participating child, supporting the promoted intervention.
The differential of the proposed methodology using the Multiple Baseline Design (Gast & Ledford, 2014) for collecting and measuring the effects of the intervention is precisely to allow the identification of advances and redirecting paths in favor of the child’s autonomy in order to accomplish the target activity. As evidenced in the study, the intervention performed did not reach the clinically significant rates of change in the PEDI evaluation, but the results indicated that the intervention produced positive effects on the child’s functional capacity. In this study, it was possible to see a gradual reduction in the level of assistance as interventions, training, and resource use were implemented, until the child reached an expected level to switch among activities to be learned, producing evidence on the intervention performed.
The implementation of devices for postural support (seat and footrest) were essential for functional independence, favoring new opportunities for the child, which, prior to the use of the resource, was not able to perform. In this sense, it is important to use resources and small improvements to assist in the execution of the activity, thus allowing the participation of the child, and consequently reducing the amount of help and assistance requested by the child. Thus, the beneficial effects of the use of an adjustable seat as well as eating and drinking utensils have been reported, supporting previous studies that show that adapted seating, as well as other AT devices, can promote eating skills and reduce the support offered for a child with functional limitations (Ostensjo, Carlberg, & Vollestad, 2005; Scherer, Craddock, & Mackeogh, 2010).
Due to the neuromotor alterations of the child, adaptations were proposed in which he did not need to hold and/or raise the glass to the mouth to drink, and different cup models were tested until finding one that was suitable for the child’s posture. After implementing the use of the glass, the child himself was finding ways to use the resource, adapting it to perform the action in an increasingly independent and comfortable way. Similarly, it was necessary to think of solutions for greater independence in the use of cutlery, since different resources were part of the test and agreements were necessary for the child to accept using some of them. It was often necessary to accept his refusal, such as the Neoprene abductor thumb brace that the child had and did not like to wear, despite pointing to better functional gain from grasping objects. In this sense, it is important to respect the user’s choices, thus allowing the use of the resource to be used on a daily basis and reducing the chances of its abandonment (Cruz, Emmel, Manzini, & Mendes, 2016; Van Niekerk, Dada, Tönsing, & Boshoff, 2017).
During the resource use intervention process, the child needed to be stimulated and motivated to perform the activity, since oral-motor dysfunction is associated with the length of feeding time for children with cerebral palsy, and thus its implementation intensifies even more the activity duration, which can generate fatigue and frustration. To minimize the negative effects, it is important to respect the process experienced by the child and promote his/her satisfaction in order to reduce the learning pressure, ensuring a pleasant, warm and stimulating environment, resulting in his/her participation and consequent reduction of care intensity for the action (Ostensjo, Carlberg, & Vollestad, 2005; Cook & Polgar, 2015).
In addition to the child’s adherence to the implementation, it is important to include the family that will reinforce its use and encourage him/her. It was possible to identify the change in the mother’s perception of the child during the intervention regarding her child’s occupational performance. She began to respect and wait for the child’s own process, favoring the activity, reducing the pressure and, consequently, reducing the intensity of care and her interference. Through the social validation questionnaire, it was possible to see the mother’s adherence throughout the resource implementation process, which reinforced its use at different times of the research collection and played an important supporting role in assisting in this learning stage, giving support and motivation, without putting pressure on the child and making the activity stressful (Ostensjo, Carlberg, & Vollestad, 2005). Still, the data obtained directly from the mother, at the end of the intervention, positively highlighted the results achieved, reiterating the importance of taking into account the demands brought by families and caregivers about the priority demands which need to be addressed (Brandão, Oliveira, & Mancini, 2014; Eard et al., 2018).
In this sense, it is emphasized that the intervention in the home context allowed more involvement of the child and his mother in the activity, meeting the considerations put by Cook and Polgar (2015), Cowan and Khan (2005) and the findings of Van Niekerk et al. (2017), who reiterate that the implementation of AT resources should always involve the child and the family, always thinking about the context, willingness, personal functional needs, understanding and respecting the individuality and particularity of the family.
5 Conclusions
It is considered that the results of the study reach the objective that was set, since it proposed and evaluated the process of implementing Assistive Technology resources for feeding activity with a child with cerebral palsy. The findings confirm the hypothesis raised by describing that home intervention allows professionals to organize the intervention with equipment that shows how the feeding activity is actually performed in the daily life of the child and his/her family, which may favor the resources remaining in use and contribute to the child’s autonomy. In addition, it is assumed that the systematic monitoring of the child’s performance during the task and each resource change constitutes an important way to support decision making about the most appropriate resources for the case.
Due to the gap identified in the literature about the lack of more specific studies on how the professional can perform the step-by-step process of implementing these resources in the context of activities of daily living and the low number of productions that support decision-making practice regarding the prescription itself of Assistive Technology resources, this study may contribute to the production of knowledge in the area, more specifically regarding the implementation of different resources for children with cerebral palsy, indicating ways and decisions taken through the child’s response. The procedures adopted to collect and systematize the child’s performance with each resource change brings evidence about the effectiveness in the intended activity, which contributes as an example for professionals dedicated to this type of intervention.
Continuity studies with a larger number of children with cerebral palsy are suggested in order to experiment with new resources and new life contexts, as well as longitudinal studies to verify whether the implemented resources are still in use by the children and their families. It is considered that the study may contribute to the knowledge that has been produced in the area, but it is important to highlight its limitations due to the small number of research participants and the short implementation period of the resource considering the participant’s difficulties.
2This work is part of the first author’s Scientific Initiation, funded by the Programa de Apoio ao Docente Recém-Doutor (Support Program for the Recent-Doctor Professor) of the Dean of Research of the Federal University of São Carlos (PADRD/PROPq/UFSCar) 2015-2017, under the guidance of the other authors. Preliminary parts of this study were presented and published as summaries at the 14th Brazilian Congress of Occupational Therapy (2016) and at the Conference of the Council of Occupational Therapists for the European Countries (2016).
REFERENCES
Brandão, M. B., Oliveira, R. H. S., & Mancini, M. C. (2014). Functional priorities reported by parents of children with cerebral palsy: contribution to the pediatric rehabilitation process. Braz. J. Phys. Ther, 18(6), 563-571. [ Links ]
Cook, A. M., & Polgar, J. M. (2015). Assistive technologies: principals and practice. St. Louis, Missouri: Mosby. [ Links ]
Copley, J., & Ziviani, J. (2004). Barriers to the use of assistive technology for children with multiple disabilities. Oc. Ther. Inter., 11(4), 229-243. [ Links ]
Cowan, D. M., & Khan, Y. (2005). Assistive technology for children with complex disabilities. Current Paediatrics, 15, 207-212. [ Links ]
Cruz, D. M. C., Emmel, M. L. G., Manzini, M. G., & Mendes, P. V. B. (2016). Assistive Technology Accessibility and Abandonment: Challenges for Occupational Therapists. The Open Journal of Occupational Therapy, 4(10). [ Links ]
Cury, V. C. R., & Brandão, M. B. (2011). Tecnologia Assistiva. In V. C. R. Cury, & M. B. Brandão, Reabilitação em Paralisia Cerebral (pp. 247-282). Rio de Janeiro: Medbook. [ Links ]
Earde, P. T., Praipruk, A., Rodpradit, P., & Seanjumla, P. (2018). Facilitators and Barriers to Performing Activities and Participation in Children with Cerebral Palsy: Caregivers’ Perspective. Pediatr. Phys. Ther., 30(1), 27-32. [ Links ]
Fachinetti, T. A, Gonçalves, A. G., & Lourenço, G. F. Processo de Construção de Recurso de Tecnologia Assistiva para Aluno com Paralisia Cerebral em Sala de Recursos Multifuncionais.Revista Brasileira de Educação Especial, 23(4), 547-562. [ Links ]
Gast, D. L., & Ledford, J. R. (2014). Single case research methodology: applications in special educational and behavioral sciences. New York: Routledge. [ Links ]
Guerzoni, V. P. D., Barbosa, A. P., Borges, A. C. C., Chagas, P. S. C., Gontijo, A. P. B., Eterovick, F., & Mancini, M. C. (2008). Análise das intervenções de terapia ocupacional no desempenho das atividades de vida diária em crianças com paralisia cerebral: uma revisão sistemática da Literatura. Rev. Bras. Saúde Matern. Infant., 8(1), 17-25. [ Links ]
Hiratuka, E., Matsukura, T. S., & Pheifer, L. I. (2010). Adaptação transcultural para o Brasil do Sistema de Classificação da Função Motora Grossa (GMFCS). Brazilian Journal of Physical Therapy, 14 (6), 537-544. [ Links ]
Iyer, L.V., Haley, S. M., Watkins, M. P., & Dumas, H. M. (2003). Establishing minimal clinically important differences for scores on the Pediatric Evaluation of Disability Inventory for inpatient rehabilitation. Physical Therapy, 83(10), 888-898. [ Links ]
Mancini, M. C. (2005). Inventário de avaliação pediátrica de incapacidade (PEDI): Manual da versão brasileira adaptada. Belo Horizonte: UFMG. [ Links ]
Mancini, M. C., Alves, A. C. M., Schaper, C., Figueiredo, E. M., Sampaio, R. F., Coelho, Z. A. C., & Tirado, M. G. A. (2004). Gravidade da Paralisia Cerebral e Desempenho funcional. Rev. Bras. Fisioter, 8(3), 253-260. [ Links ]
Monteiro, J. A., Vasconcelos, T. B., Silva, R. L. M., & Cavalcante, L. I. C. (2012). Avaliação do nível de independência nas atividades de vida diária da criança com paralisia cerebral: um estudo de caso. Cad. Ter. Ocup. UFSCar, 20(1), 129-141. [ Links ]
Novak, I., Smithers-Sheedy, H., & Morgan, C. (2012). Predicting equipment needs of children with cerebral palsy using the Gross Motor Function Classification System: a cross-sectional study. Disability & Rehabilitation: Assistive Technology, 7(1), 30-36. [ Links ]
Ostensjo, S., Carlberg, E. B., & Vollestad, N. K. (2005). The use and impact of assistive devices and other environmental modifications on everyday activities and care in young children with cerebral palsy. Disability and Rehabilitation, 27(14), 849-861. [ Links ]
Pfeifer, L. I., Silva, D. B. R., Lopes, P. B., Matsukura, T. S., Santos, J. L. F., & Pinto, M. P. P. (2014). Social support provided to caregivers of children with cerebral palsy.Child: care, health and development, 40(3), 363-369. [ Links ]
Scherer, M. J., Craddock, G., & Mackeogh, T. (2010). The relationship of personal factors and subjective well-being to the use of assistive technology devices. Disability and Rehabilitation, 33(10), 811-817. [ Links ]
Silva, D. B. R., Pfeifer, L. I., & Funayama, C. A. R. (2010a). GMFCS - E & R Sistema de Classificação da Função Motora Grossa Ampliado e Revisto. Recuperado em 20 de setembro de 2019 de https://canchild.ca/system/tenon/assets/attachments/000/000/075/original/GMFCS-ER_Translation-Portuguese2.pdf [ Links ]
Silva, D. B. R., Pfeifer, L. I., & Funayama, C. A. R. (2010b). Sistema de classificação de habilidade manual para crianças com paralisia cerebral 4-18 anos. Recuperado em 20 de setembro de 2019 de www.macs.nu [ Links ]
Silva, J. M., & Araujo, T. C. C. F. (2019). Reabilitação pediátrica: Suporte social e estresse em casos de paralisia cerebral.Psicologia: Teoria e Prática, 21(1), 119-136. [ Links ]
Silva, S. S. C., & Pontes, F. A. R. (2016). Rotina de famílias de crianças com paralisia cerebral.Educar em Revista, 59, 65-78. [ Links ]
Sposito, M. M. M., & Riberto, M. (2010). Avaliação da funcionalidade da criança com paralisia cerebral espástica. Acta Fisiatr., 17(2), 50-61. [ Links ]
Tromby, C. A., & Radomski, M. V. (2005). Terapia Ocupacional para disfunção física. São Paulo: Livraria Santos Editora. [ Links ]
Van Niekerk, K., Dada, S., Tönsing, K., & Boshoff, K. (2017). Factors Perceived by Rehabilitation Professionals to Influence the Provision of Assistive Technology to Children: A Systematic Review. Physical & Occupational Therapy In Pediatrics, 38(2), 168-189. [ Links ]
Watson, A. H., Ito, M., Smith, R. O., & Anderson, L. T. (2010). Effect of assistive technology in a public-school setting. American Journal of Occupational Therapy, 64(1), 18-29. [ Links ]
Windholz, M. H. (2016). Passo a passo seu caminho: guia curricular para ensino de habilidades básicas. São Paulo: Edicon. [ Links ]
Received: April 02, 2019; Revised: September 09, 2019; Accepted: September 12, 2019











 texto em
texto em 



