Serviços Personalizados
Journal
Artigo
Compartilhar
Revista Brasileira de Educação Especial
versão impressa ISSN 1413-6538versão On-line ISSN 1980-5470
Rev. bras. educ. espec. vol.26 no.3 Marília jul./set 2020 Epub 12-Ago-2020
https://doi.org/10.1590/1980-54702020v26e0109
Research Report
Developmental Motor Scale: Adaptation for Children with Low Vision from 7 to 10 Years Old
2Mestre em Fisioterapia pelo Programa de Pós-Graduação em Fisioterapia, Universidade Federal do Triângulo Mineiro. Uberaba/Minas Gerais/Brasil. E-mail: ceciliacarizzi@gmail.com.
3Professora associada ao Departamento de Fisioterapia Aplicada, Universidade Federal do Triângulo Mineiro, Uberaba, Minas Gerais, Brasil. surayagnovais@gmail.com.
4Mestre em Fisioterapia pelo Programa de Pós-Graduação em Fisioterapia, Universidade Federal do Triângulo Mineiro. Uberaba/Minas Gerais/Brasil. E-mail: nanda_izeppi@hotmail.com.
5Fisioterapeuta, graduação na Universidade Federal do Triângulo Mineiro. Uberaba/Minas Gerais/Brasil. E-mail: larissagiovanna2009@hotmail.com.
6Mestranda em Fisioterapia pelo Programa de Pós-Graduação em Fisioterapia, Universidade Federal do Triângulo Mineiro. Uberaba/Minas Gerais/Brasil. E-mail: paulabertelip@hotmail.com.
7Professora associada ao Departamento de Fisioterapia Aplicada e do Programa de Pós-Graduação em Fisioterapia, Universidade Federal do Triângulo Mineiro. Uberaba/Minas Gerais/Brasil. E-mail: karina.pereira@uftm.edu.br.
Low vision is a type of visual impairment that can influence the child’s functionality and cause important changes in the acquisition of motor skills during childhood. The objective of this paper was to evaluate the reliability aspects in the adaptation of the Developmental Motor Scale (PDMS) for children with low vision, from 7 to 10 years of age. Twenty-two children with low vision (± 9.12 years) participated in the study. The scale was adapted in four stages. To analyze the agreement between the judges’ answers, the agreement index (≥ 80%) was used, and for the reliability of the adaptations the inter-rater and retest analysis was used (Intraclass Correlation Coefficient). The results showed that the agreement rate between the judges was ≥80% in the second round of adaptations, which showed excellent reliability in the inter-rater analysis (ICC≥1,000) and in the retest test (ICC≥0,990) for the motor age, and excellent inter-rater reliability (ICC≥1,000) and in the retest test (ICC≥0.997) for the motor quotient. The PDMS was adapted and presented good methodological reliability. Thus, its adaptation will allow the correct use of the instrument in children with low vision, determining the most accurate functional/motor diagnosis of motor alterations in this population.
KEYWORDS: Special Education; Vision disturbances; Child; Rating Scale; Adaptation
A baixa visão é um tipo de deficiência visual que pode influenciar na funcionalidade da criança e ocasionar alterações importantes na aquisição das habilidades motoras na infância. O objetivo deste artigo foi avaliar os aspectos de confiabilidade na adaptação da Escala de Desenvolvimento Motor (EDM) para crianças com baixa visão, dos 7 aos 10 anos de idade. Participaram do estudo 22 crianças com baixa visão (± 9,12 anos). A adaptação da escala ocorreu em quatro etapas. Para analisar a concordância entre as respostas dos juízes, foi utilizado o índice de concordância (≥ 80%) e, para a confiabilidade das adaptações, utilizou-se a análise inter-avaliador e reteste (Coeficiente de Correlação Intraclasse). Os resultados demonstraram que o índice de concordância entre os juízes foi ≥80% na segunda rodada de adaptações, as quais mostraram excelente confiabilidade na análise interavaliadores (CCI≥1,000) e no teste reteste (CCI≥0,990) para a idade motora, e excelente confiabilidade interavaliadores (CCI≥1,000) e no teste reteste (CCI≥0,997) para quociente motor. A EDM foi adaptada e apresentou boa confiabilidade metodológica. Assim, sua adaptação permitirá o uso correto do instrumento em crianças com baixa visão, determinando o diagnóstico funcional/motor mais preciso das alterações motoras nessa população.
PALAVRAS-CHAVE: Educação Especial; Distúrbios da visão; Criança; Escala de avaliação; Adaptação
1 Introduction
Vision is extremely important in capturing information from the environment, being fundamental to the child development process (World Health Organization [WHO], 2013). Visual disorders generate a decrease in exteroceptive information, presenting itself in a reduced form and causing the restriction of motor experiences (Santos, Passos, & Rezende, 2007).
Children with low vision show qualitative and quantitative differences in the acquisition of motor skills when compared to children with normal vision (Uysal & Düger, 2011). In addition, alterations in gross and fine motor skills are observed (Bouchard & Tétreault, 2000), orthostatic balance, speed of postural adjustment (Matos, Matos, & Oliveira, 2010) and gait parameters (Hallemans, Ortibus, Meire, & Aerts, 2010).
The motor development of children with low vision can be satisfactory with motor intervention programs and physical activities (Houwen, Visscher, Lemmink, & Hartman, 2009; Jazi, Purrajabi, Movahedi, & Jalali, 2012). For that, a careful evaluation with adapted instruments and tasks in order to identify the child’s motor development level is important.
In Brazil, the instrument for assessing motor performance, called Movement Assessment Battery for Children-2 (MABC-2), was adapted, and the modifications were validated for children with low vision from 7 to 10 years of age (Bakke, Sarinho, & Cattuzzo, 2017). In the Netherlands, the Test of Gross Motor Development (TGMD-2) (Houwen, Hartman, Jonker, & Visscher, 2010) was adapted for children with low vision from 6 to 12 years old. In the studies conducted by Schmitt and Pereira (2014, 2016), the authors made cubes with luminous stimulus and high contrast (black and white) to help categorize the motor actions of children with low vision. However, it is observed that the adapted MABC-2 (Bakke, Sarinho, & Cattuzzo, 2017) - the only adapted instrument that had its modifications validated for Brazilian children with low vision - aimed at the analysis of motor performance. The scale encompasses important domains, but which refer only to manual dexterity, pointing and receiving, as well as balance, which indicates the need for adaptation to broader motor development evaluation instruments.
In this sense, this study aims to contribute to this area of interest by adapting another evaluation tool for children with low vision that identifies motor age in various psychomotor aspects, such as the Motor Development Scale (PMDS) (Rosa Neto, 2015), validated in Brazil. The adaptation of this scale will establish appropriate strategies and conduct for the rehabilitation of visually impaired children, in addition to their inclusion in their environmental context. In this perspective, the objective of this study was to evaluate the aspects of reliability in the adaptation of the Motor Development Scale (PMDS) for children from 7 to 10 years of age with low vision.
2 Methods
This is a methodological study of adaptation of instruments, approved by the Research Ethics Committee (2.152.730/2017). For the process of adapting the PDMS, three children with low vision participated, with an average age of 105.7 months (±8.08). Nineteen children with low vision, eleven girls, with an average age of 110.8 months (±9.23), participated in the process of reliability of the adaptations. These belonged to different schools specializing in the care of visually impaired children in the Triângulo Mineiro, located in the state of Minas Gerais, Brazil and in the interior of São Paulo, Brazil. The sample selection was intentional and children with neurological disorders, orthopedic alterations, behavioral problems and hearing loss were not included.
PDMS’s adaptation was authorized by the author, Professor Francisco Rosa Neto. Initially, three children with low vision were evaluated with the original PDMS to obtain their responses to the applied motor tests (pre-test). The adaptation took place in four stages (Figure 1).
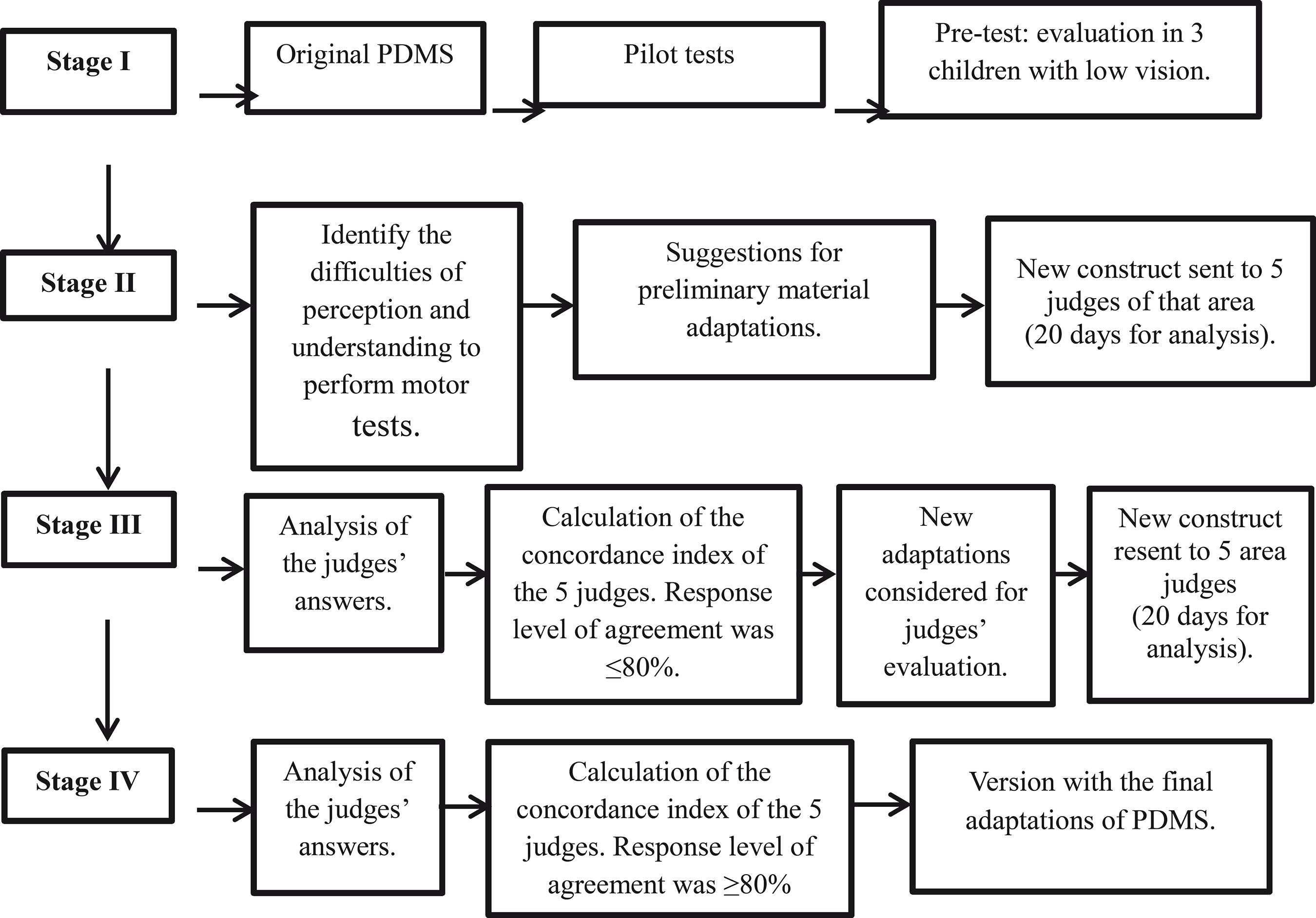
Source: Elaborated by the authors.
Figure 1 Flowchart of the process of adapting the PDMS for children with low vision from 7 to 10 years of age.
The first stage consisted of the footage analysis by four researchers with experience in the application of the scale and in the rehabilitation of children with low vision, in which they identified and recorded, by consensus, the greatest difficulties observed during the performance of the PDMS tests. In the second stage, preliminary adaptations were proposed in some PDMS tests (fine motor skills, global motor skills, body scheme, spatial and temporal organization) in order to favor the understanding and visual perception of the tests, without detracting from the original test proposed by the author. The adaptations were presented in tables and sent with guidance on the evaluation of adaptations to five other judges with previous experience in the area of visual impairment and child rehabilitation. The judges should mark I agree “A” or I do not agree “NA” in each test presented. If the answer was negative, they should suggest a new adaptation. The third stage consisted of analyzing the responses of the five judges; in this case, some did not agree and suggested new adaptations. These adaptations were accepted by the researchers and a new table was prepared and sent back to the same judges, following the previous criteria. In the fourth stage, the judges sent small suggestions and an agreement was reached between them in the amount of ≥80% (Polit & Beck, 2006).
The adaptations of PDMS materials were mainly related to the use of color contrasts and textures of objects (black, white, yellow, colored glue, white masking tape and black non-slip tape, among others), lighting (luminaire with 60W lamp), suitable materials and of common use for visual impairment (such as pencil 6B).
At the end of the adaptations, the reliability of the adapted PDMS was applied, through the evaluation of 19 children with low vision by two evaluators simultaneously. After 15 days, the same children were reevaluated by a single evaluator, in order to increase the reliability of the instrument.
For the statistical analysis of inter-rater reliability and test-retest, the Intraclass Correlation Coefficient (ICC) was used. These analyzes were performed in the calculations of the motor age of each task, in the general motor age, in the motor quotients of each task and in the general motor quotient. The significance level of p≤0.05 was considered.
3 Results
Table 1 shows the sequence of agreement between the judges to adapt the scale.
Table 1 Result of the adaptation process in the two rounds of evaluations by the judges.
| FINE MOTRICITY | |||||||||||||||
| AGE | TASK | ADAPTATION STAGE I | SUGGESTIONS FROM EXPERTS | IA | FINAL ADAPTATION RESEARCHERS | SUGGESTIONS FROM EXPERTS | IA | ||||||||
| 5 years old | Make a knot | No adaptations. Use of lamp on the activity table. | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| A | A | A | A | Yellow cord, black pencil NA | 80% | Maintained | A | A | A | A | A | 100% | |||
| 6 years old | Maze | Modify the drawing size. Expanded to 1 cm. Use of lamp. | Increase line thickness NA | Reel and increase line thickness NA | Increase line thickness NA | Increase line thickness NA | Use of pencil 6B NA | WA | The drawing was enlarged by 1 cm and the thickness of the drawing line by 1 cm. Pencil 6B. | A | A | A | A | A | 100% |
| 7 years old | Paper balls | Add black EVA sheet (30 x 30). Use of lamp. | A | A | A | A | A | 100% | Maintained | A | A | A | A | A | 100% |
| 8 years old | Thumb tip | The examiner will make the demonstration at a 30 cm distance from the child's face. | A | Child to feel the evaluator's hand. NA | A | A | A | 80% | The examiner will make the demonstration at a 30 cm distance from the child's face. Child feels the evaluator's hand. | A | A | A | A | A | 100% |
| 9 years old | Throwing a ball | Add a black EVA sheet (30 x 30) behind the yellow target (contrast). | A | Non-slip texture to delimit the child's distance. NA | A | A | A | 80% | Maintained | A | Rattle ball NA | A | A | A | 80% |
| 10 years old | Circle with thumb | The examiner will make the demonstration at a 30 cm distance from the child's face. | A | Child to feel the evaluator's hand. NA | Glove with color contrast in the evaluator's hand, demonstration to the child. NA | A | A | 60% | The examiner will make the demonstration at a 30 cm distance from the child's face. Child feels the evaluator's hand. | A | A | A | A | A | 100% |
| 11 years old | Grab a ball | Ball with contrasting color and rattle. | A | A | A | Rattle (distract child's attention) NA | A | 80% | Color contrast ball (yellow and black) | A | Rattle ball NA | A | A | A | 80% |
| GLOBAL MOTRICITY | |||||||||||||||
| AGE | TASK | ADAPTATION STAGE I | SUGGESTIONS FROM EXPERTS | IA | FINAL ADAPTATION RESEARCHERS | SUGGESTIONS FROM EXPERTS | IA | ||||||||
| 5 years old | Jump from a height of 20 cm. | Black EVA on the floor, child safety and color contrast. | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| 2 cm high EVA rubberized mat or tatami mat. NA | A | A | A | A | 80% | 2 cm high rubberized EVA mat. | A | A | A | A | A | 100% | |||
| 6 years old | Walk on a straight line | Contrast yellow and black stripe | A | Non-slip tape, child feels the line. NA | Textured tape, barefoot child, smooth sandpaper with contrast. NA | A | A | 60% | Textured non-slip tape, smooth sandpaper, black in contrast to white adhesive tape on the side edges (3 meters). | A | A | A | A | A | 100% |
| 7 years old | Lame Foot | Contrast yellow and black stripe | A | Non-slip tape, demarcation on the floor stripe of 15cm. NA | Textured tape, barefoot child, smooth sandpaper with contrast. NA | A | A | 60% | Textured non-slip tape, smooth sandpaper, black in contrast to white adhesive tape on the side edges (3 meters). | A | A | A | A | A | 100% |
| 8 years old | Jump from a height of 40 cm. | Black EVA on the floor, child safety and color contrast. | 2 cm high EVA rubberized mat or tatami mat. NCA | A | A | A | A | 80% | 2 cm high rubberized EVA mat. | A | A | A | A | A | 100% |
| 9 years old | Jumping in the air | The original application of the test was maintained | A | A | A | A | A | 100% | Maintained | A | A | A | A | A | 100% |
| 10 years old | Lame foot with wooden rectangle | Contrast yellow and black stripe Wooden rectangle in black and white contrast. | Single color rectangle (white) NA | Black textured tape, single color rectangle (white) NA | A | A | A | 60% | Textured non-slip tape, smooth sandpaper, black in contrast to white adhesive tape on the side edges (3 meters). | A | A | A | A | A | 100% |
| 11 years old | Jumping over a chair | The original application of the test was maintained | Contrast color tapes on the chair seat. NA | Child to feel the height of the seat, with color contrast. NA | A | A | A | 60% | Yellow EVA on the chair seat, child feels the height of the chair. | A | A | A | A | A | 100% |
| BODY SCHEME | |||||||||||||||
| AGE | TASK | ADAPTATION STAGE I | SUGGESTIONS FROM EXPERTS | IA | FINAL ADAPTATION RESEARCHERS | SUGGESTIONS FROM EXPERTS | IA | ||||||||
| 2 - 5 years old | Test of imitation of simple gestures (hand movements). Test of imitation of simple gestures (movements with arms). | The original application of the test was maintained. | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| Make the evaluation at a 30 cm distance from the child's face. NA | Make the evaluation at a 30 cm distance from the child's face, allow to feel the movement. NA | Gloves with color contrast. NA | A | A | 40% | Make the evaluation at a 30 cm distance from the child's face, allow to feel the movement. | A | A | A | A | A | 100% | |||
| 6 - 11 years old | Speed Test | Use of pencil 6B. | Enlarge the checkerboard design of the sheet. NA | Child reel to feel the drawing, increase the thickness of the lines, child to feel the drawing. NA | Increase the line thickness of the drawing. NA | High contrast lines | A | 20% | The checkered line in the drawing was increased to 1 cm, the reel was used in the drawing lines, the child was allowed to feel the drawing. | A | A | A | A | A | 100% |
| SPATIAL ORGANIZATION | |||||||||||||||
| AGE | TASK | ADAPTATION STAGE I | SUGGESTIONS FROM EXPERTS | IA | FINAL ADAPTATION RESEARCHERS | SUGGESTIONS FROM EXPERTS | IA | ||||||||
| 5 years old | Solitaire Game | Black EVA 30 × 30 under the cards (blue and yellow, originals of the test). | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| A | A | A | A | A | 100% | Black EVA 30 × 30 under the cards (blue and yellow, originals of the test). | A | A | A | A | A | 100% | |||
| 6 years old | Knowing yourself | The original application of the test was maintained. | A | A | A | A | A | 100% | The original application of the test was maintained. | A | A | A | A | A | 100% |
| 7 years old | Execution of right and left movements | The original application of the test was maintained. | A | A | A | A | A | 100% | The original application of the test was maintained. | A | A | A | A | A | 100% |
| 8 years old | Recognition about the other | Contrasting yellow and black ball. | A | A | A | A | A | 100% | Contrasting yellow and black ball. | A | (rattle in the ball) NA | A | A | A | 80% |
| 9 years old | Human reproduction | The original application of the test was maintained. | A | A | Black glove with color contrast, approach at 30 cm from the child's face. NA | A | A | 80% | The original application of the test was maintained | A | A | A | A | A | 100% |
| 10 years old | Schematic Dummy | Black EVA under the cards for color contrast, figures in high relief so that the child can touch and visualize the dummies, present at 30cm distance from the child's face. | A | A | A | A | A | 100% | Black EVA under the cards for color contrast, figures in high relief so that the child can touch and visualize the dummies, present at 30cm distance from the child's face. | A | A | A | A | A | 100% |
| 11 years old | Position of three objects. | Change the colors of the cubes to black and white. | Color contrast cubes. NA | Color contrast cubes. NA | A | background NA | A | 40% | Contrasting color cubes (black and white, yellow and red and yellow and black). | A | A | A | A | A | 100% |
| TEMPORAL ORGANIZATION | |||||||||||||||
| AGE | TASK | ADAPTATION STAGE I | SUGGESTIONS FROM EXPERTS | IA | FINAL ADAPTATION RESEARCHERS | SUGGESTIONS FROM EXPERTS | IA | ||||||||
| 2 - 5 years old | Expressive language | The original application of the test was maintained. | 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||
| A | A | A | A | A | 100% | The original application of the test was maintained. | A | A | A | A | A | 100% | |||
| 6 - 11 years old | Stage 1 (Sound reproduction) | The original application of the test was maintained. | A | A | A | A | A | 100% | The original application of the test was maintained. | A | A | A | A | A | 100% |
| Stage 2 (Symbolization, design of spatial structures). | Add black EVA under the cards for color contrast, high relief figures for children to view the images. | Make only circles and not faces. NA | Using cardboard, child draws, instead of EVA the child feels the image. NA | A | A | A | 60% | Add black EVA under the cards for color contrast, figures in high relief for children to view the images (circles). | A | A | A | A | A | 100% | |
| Stage 3 (Symbolization of temporal structures). | Add black EVA under the cards for color contrast, high relief figures for children to view the images. | Make only circles and not faces. NA | Make only circles and not faces. NA | A | A | A | 60% | Add black EVA under the cards for color contrast, figures in high relief for children to view the images (circles). | A | A | A | A | A | 100% | |
| Stage 4 Transcription of temporal structures (dictated). | The original application of the test was maintained. | A | A | A | A | A | 100% | Add black EVA under the cards for color contrast, figures in high relief for children to view the images (circles). | A | A | A | A | A | 100% | |
Source: Elaborated by the authors.
Legend: IA - index of agreement between the judges; NA - does not agree, A - agrees, WA - without agreement.
Based on the agreement between the judges in the adaptation process, the construction of materials adapted from the PDMS began (Figure 2).

Figure 2 Image of the instrument and the final adaptations of the PDMS. Legend: Image of the original instrument (A) and the final adaptations (B) of PDMS.
When analyzing the motor age and general motor age scores, excellent inter-rater reliability (ICC≥1,000) and test-retest (ICC≥0.990) is noted in all motor tasks (p=0.001). At motor ages IM2, IM5 and IM6, the variance was zero, that is, the evaluators’ scores were the same in these motor tasks (Table 2).
Table 2 Inter-rater reliability and test-retest (ICC) of the MA and GMA obtained in the motor tests.
| Motor age |
EVALUATOR 1 (PQ1) | EVALUATOR 2 (PQ2) | RETEST (RET) | ICC | p Value | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | MED | SD | MIN | MAX | M | MED | SD | MIN | MAX | M | MED | SD | MIN | MAX | RS1/RS2 | RS1/RET | RS1/RS2 | RS1/RET | |
| MA1 | 108,00 | 108,00 | 14,56 | 84,00 | 132,00 | 108,00 | 108,00 | 14,06 | 84,00 | 132,00 | 110,00 | 108,00 | 14,17 | 84,00 | 132,00 | 0,995 | 0,959 | 0,001 | 0,001 |
| MA2 | 105,00 | 108,00 | 12,38 | 72,00 | 132,00 | 105,00 | 108,00 | 12,38 | 72,00 | 132,00 | 107,00 | 108,00 | 13,54 | 72,00 | 132,00 | 1,000 | 0,888 | _ | 0,001 |
| MA3 | 93,16 | 96,00 | 27,30 | 48,00 | 132,00 | 91,89 | 96,00 | 29,12 | 48,00 | 132,00 | 96,32 | 108,00 | 25,80 | 48,00 | 132,00 | 0,990 | 0,973 | 0,001 | 0,001 |
| MA4 | 61,89 | 60,00 | 10,78 | 48,00 | 96,00 | 60,00 | 60,00 | 8,00 | 48,00 | 72,00 | 65,05 | 60,00 | 10,81 | 48,00 | 96,00 | 0,707 | 0,843 | 0,001 | 0,001 |
| MA5 | 89,05 | 84,00 | 10,81 | 72,00 | 108,00 | 89,05 | 84,00 | 10,81 | 72,00 | 108,00 | 93,47 | 96,00 | 11.01 | 72,00 | 120,00 | 1,000 | 0,793 | _ | 0,001 |
| MA6 | 115,58 | 120,00 | 19,27 | 72,00 | 132,00 | 115,58 | 120,00 | 19,27 | 72,00 | 132,00 | 116,21 | 132,00 | 19,61 | 72,00 | 132,00 | 1,000 | 0,990 | _ | 0,001 |
| GMA | 95,53 | 94,00 | 7,84 | 82,00 | 109,00 | 95,05 | 94,00 | 8,29 | 80,00 | 109,00 | 98,11 | 96,00 | 7,63 | 84,00 | 111,00 | 0,985 | 0,938 | 0,001 | 0,001 |
Source: Elaborated by the authors.
Legend:MA = motor age; MA1 - motor age of fine motor skills, MA2 - motor age of global motor skills, MA3 - motor age of balance, MA4 - motor age of body scheme, MA5 - motor age of spatial organization, MA6 - motor age of temporal organization, GMA = general motor age; M = mean; MED = median; SD = standard deviation; MIN = minimum; MAX = maximum, ICC = intraclass correlation coefficient, RS1/RS2 = researcher 1 and 2, RS1/RET = researcher 1 and retest, p = p value.
In the analysis of the motor quotients and general motor quotient, the values were also excellent in the inter-rater reliability (ICC≥1,000) and in the test-retest (ICC≥0.997) in all motor tasks of the scale (p=0.001). In QM6, the variance was zero, that is, the evaluators’ score was the same in this motor test (Table 3).
Table 3 Inter-rater reliability and test-retest (ICC) of the motor quotient and the general motor quotient.
| M | MED | SD | MIN | MAX | M | MED | SD | MIN | MAX | M | MED | SD | MIN | MAX | RS1/RS2 | RS1/RET | RS1/RS2 | RS1/RET | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MQ1 | 98,58 | 103,00 | 15,33 | 73,00 | 127,00 | 99,05 | 103,00 | 15,20 | 73,00 | 127,00 | 99,42 | 103,00 | 15,46 | 74,00 | 127,00 | 0,995 | 0,997 | 0,001 | 0,001 |
| MQ2 | 96,05 | 95,00 | 13,85 | 66,00 | 120,00 | 96,21 | 95,00 | 13,97 | 66,00 | 120,00 | 96,74 | 95,00 | 13,81 | 65,00 | 118,00 | 0,999 | 0,933 | 0,001 | 0,001 |
| MQ3 | 83,58 | 92,00 | 20,87 | 38,00 | 112,00 | 82,37 | 92,00 | 22,65 | 38,00 | 112,00 | 85,84 | 92,00 | 19,35 | 37,00 | 110,00 | 0,982 | 0,958 | 0,001 | 0,001 |
| MQ4 | 56,84 | 53,00 | 14,38 | 37,00 | 98,00 | 55,00 | 52,00 | 11,29 | 38,00 | 79,00 | 59,32 | 60,00 | 14,98 | 36,00 | 98,00 | 0,852 | 0,925 | 0,001 | 0,001 |
| MQ5 | 81,58 | 81,00 | 15,06 | 56,00 | 112,00 | 81,68 | 81,00 | 14,98 | 56,00 | 112,00 | 84,47 | 82,00 | 13,38 | 64,00 | 112,00 | 1,000 | 0,921 | 0,001 | 0,001 |
| MQ6 | 103,68 | 109,00 | 24,22 | 60,00 | 145,00 | 103,68 | 109,00 | 24,22 | 60,00 | 145,00 | 105,21 | 106,00 | 21,62 | 65,00 | 141,00 | 1,000 | 0,911 | _ | 0,001 |
| QMG | 87,49 | 88,98 | 10,24 | 71,00 | 103,00 | 87,99 | 88,98 | 11,14 | 71,00 | 109,00 | 88,97 | 89,11 | 10,15 | 72,00 | 104,00 | 0,926 | 0,985 | 0,001 | 0,001 |
Source: Elaborated by the authors.
Legend: MQ = motor quotient; MQ1 - motor quotient of fine motor skills, MQ2 - motor quotient of global motor skills, MQ3 - motor quotient of balance, MQ4 - motor quotient of body scheme, MQ5 - motor quotient of spatial organization and MQ6 - motor quotient of temporal organization, QMG = general quotient motor; M = mean; MED = median; SD = standard deviation; MIN = minimum; MAX = maximum, ICC = intraclass correlation coefficient, RS1/RS2 = researcher 1 and 2, RS1/RET = researcher 1 and retest, p = p value.
4 Discussion
The outcomes of the adaptations of the PDMS for children with low vision from 7 to 10 years of age showed that the modifications made to the instrument were suitable for the tests’ batteries, in view of the good agreement index among the judges.
The study methodology adopted strict criteria to evaluate the adaptations made in the motor tests of the instrument’s test batteries. Note that clinical observation is very important for the adaptation of instruments; however, it must be accompanied by the opinion of judges, a fundamental resource, which considerably influences the generation of appropriate items for the construction of scales (Keszei, Novak, & Streiner, 2010; Streiner & Norman, 2008). This care and rigor resulted in agreement between them, in more than half of the battery tests, in the first phase of the adaptations.
Regarding the test batteries, the experts disagreed, mainly in the global motricity and in the body scheme. It is important to note that skills such as walking, jumping and leaping are directly linked to visual perception (Rosa Neto, 2015); thus, children with low vision may have deficits in these psychomotor aspects (Bouchard & Tétreaut, 2000; Uysal & Duger, 2011).
The same occurred with the body scheme, as children with low vision may have an impaired sense of the body and have difficulties in relating to spaces, objects and people around them (Boato, 2012). The judges recommended changes related to the presentation of the task so that it was performed close to the child’s face. This suggestion resulted in a better understanding of the tasks by children with visual impairments.
In the second phase of the adaptations, the researchers responded to the judges’ suggestions in the test batteries, resulting in good agreement among them, allowing the adaptation of the instrument for children with low vision, with the reliability being tested. The literature points out that evaluation instruments are useful when they present scientifically robust results, demonstrating good quality of their psychometric properties (Cano & Hobart, 2011; Coluci, Alexandre, & Milani, 2015; Souza, Alexandre, & Guirardello, 2017).
In some test batteries, the children did not have difficulties in understanding how to perform the motor tests of PDMS, as was observed in the tests of balance and laterality, in which there were small adjustments due to low vision. In this case, in the motor balance tests, the child could feel the movement in the evaluator, since, laterally, he/she could feel the object before the task was performed. Thus, it can be considered that the simplification of the environment and the task eliminates the excess of information and can assist children in the good performance of the skill (Topor, 2014).
Another highlight regarding the agreement of the judges, in the two rounds of adaptation, was the batteries of spatial organization, fine motor skills and temporal organization. In the spatial organization, adaptations were necessary only in the 11-year-old motor test (position of three objects), in relation to the color contrast of the cubes. In fine motor skills, adjustments were necessary in the motor tests of 6 and 10 years old (labyrinth and circle with the thumb). Finally, in the temporal organization, adaptations were made in stages 2 and 3 of the motor tests from 6 to 11 years old regarding the color contrast and high relief of the figures presented to the children during the tests.
Some simple adaptations were necessary, since children with low vision have difficulties related to the ability to organize temporal space (Rosa Neto, 2015) and fine motor skills, the ability being coordinated by the visual-motor action, limited in visual impairment (Haddad, 2006). Thus, the test batteries were adapted in a similar way to other modifications made in motor tests applied to children with low vision, from 7 to 10 years of age, as in the study by Bakke, Sarinho and Cattuzzo (2017) with the adaptation of MABC-2. The modified materials included the child’s use of touch, color contrast, approximation of the evaluator for demonstration of the task, increased line and drawing thickness. This shows the ease of adaptation of these instruments for children with low vision, in addition to the simplicity in the reproducibility of the tests, which should encourage researchers to adapt motor evaluation instruments for this population, in view of the scarcity in the literature and the importance in terms of accurate diagnosis of alterations in motor development.
The motor tests with the greatest disagreement among the evaluators were related to the batteries of tests of global motricity and body scheme. In global motricity, adaptations were necessary at the ages of 6, 7, 10 and 11 (walking in a straight line, lame foot, lame foot with wooden rectangle and jumping on a chair, respectively).
In the body scheme, the tests were adapted in the age range of 2 to 5 years old (imitation of simple gestures) and from 6 to 11 years old (speed test). In low vision, loss of visual acuity compromises the field of vision, decreasing the ability to perceive objects, the location, distance and depth of objects, causing alterations in spatial orientation (Sánchez, 1994). The visual function can be optimized with simple modifications such as the use of color contrast, increasing the size of objects, lighting the task, reducing the distance between the work area and the object to be manipulated, in addition to using the remaining senses (touch and hearing) (Bakke, Sarinho, & Cattuzzo, 2017; Houwen et al., 2010; Schmit & Pereira, 2014, 2016). These adjustments were necessary in the process of adapting the PDMS and helped the children to understand and perform the tasks.
The adaptations made in the PDMS resulted in good inter-rater reliability and test retest, which can assist in the reproducibility of the study in future research, since the reliability of the results allows a safe evaluation with intervention processes (Coluci, Alexandre, & Milani, 2015). PDMS is an instrument that assesses all psychomotor aspects in childhood (Rosa Neto, 2015). Its adaptation for children with low vision from 7 to 10 years of age will allow the correct use of the instrument for this specific population, will be able to determine the most accurate functional/motor diagnosis of motor alterations in low vision and assist in the appropriate intervention procedures for professionals of the area, in order to favor the full inclusion of these children in the environmental context and tasks in their daily routine. The adapted PDMS showed good reliability, so it is indicated for the evaluation of children with low vision from 7 to 10 years of age.
5 Conclusion
Considering the good methodological reliability obtained, PDMS was adapted for children with low vision from 7 to 10 years of age. PDMS is an instrument that evaluates all psychomotor aspects in childhood (Rosa Neto, 2015). Its adaptation allows the correct use of the instrument in children with low vision, in order to determine the most accurate functional/motor diagnosis of motor alterations in this population, assist in appropriate intervention procedures for professionals in the area and favor the full inclusion of these children in the context environmental and tasks in their daily routine.
Research in the area such as the adaptation of the Movement Assessment Battery for Children-2 (MABC-2) (Bakke, Sarinho, & Cattuzzo, 2017) of the Test of Gross Motor Development (TGMD-2) (Houwen et al., 2010), as well as in studies by Schmitt and Pereira (2014, 2016) demonstrated that adaptations related to color adjustment, contrast, lighting, space or distance and time can facilitate the performance of children with low vision in the performance of a motor task, which consequently will allow their motor skills to be properly characterized.
Thus, instruments for evaluating motor development assist in detecting possible alterations and collaborate in the process of motor stimulation of children with visual impairment. Adaptations in the environmental and task context are essential to allow an accurate evaluation in this population.
Referências
Bakke, H. A., Sarinho, S. W., & Cattuzzo, M. T. (2017). Adaptation of the MABC-2 Test (Age Band 2) for children with low vision. Research in Developmental Disabilities, 71, 120-129. DOI: https://doi.org/10.1016/j.ridd.2017.10.003 [ Links ]
Boato, E. M. (2012). Introdução a Educação Psicomotora: a vez e a voz do corpo na escola. Brasília: Instituto de Ensino e Pesquisa em Saúde e Educação. [ Links ]
Bouchard, D., & Tétreault, S. (2000). Motor development of sighted children and children with moderate low vision aged 8-13. Journal of Visual Impairment & Blindness, 94(9), 564-573. DOI: https://doi.org/10.1177%2F0145482X0009400903 [ Links ]
Cano, S. J., & Hobart, J. C. (2011). The problem with health measurement. Patient Prefer Adherence, 5, 279-290. DOI: https://dx.doi.org/10.2147%2FPPA.S14399 [ Links ]
Coluci, M. Z. O., Alexandre, N. M. C., & Milani, D. (2015). Construção de instrumentos de medida na área da saúde. Ciências e Saúde Coletiva, 20(3), 925-936. DOI: https://doi.org/10.1590/1413-81232015203.04332013 [ Links ]
Haddad, M. A. O. (2006). Habilitação e reabilitação visual de escolares com baixa visão: aspectos médico-sociais. Tese de Doutorado, Departamento de Oftalmologia e Otorrinolaringologia, Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brasil. [ Links ]
Hallemans, A., Ortibus, E., Meire, F., & Aerts, P. (2010). Low vision affects dynamic stability of gait. Gait & Posture, 32(4), 547-551. DOI: https://www.researchgate.net/deref/http%3A%2F%2Fdx.doi.org%2F10.1016%2Fj.gaitpost.2010.07.018 [ Links ]
Houwen, S., Visscher, C., Lemmink, K. A. P. M., & Hartman, E. (2009). Motor skill performance of children and adolescents with visual impairments: a review. Exceptional Children, 75(4), 464-492. DOI: https://doi.org/10.1177%2F001440290907500405 [ Links ]
Houwen, S., Hartman, E., Jonker, L., & Visscher, C. (2010). Reliability and Validity of the TGMD-2 in primary-school-age children with visual impairments. Adapted Physical Activity Quarterly - APAQ, 27(2), 143-159. DOI: https://doi.org/10.1123/apaq.27.2.143 [ Links ]
Jazi, S. D., Purrajabi, F., Movahedi, A., & Jalali, S. (2012). Effect of selected balance exercises on the dynamic balance of children with visual impairments. Journal of Visual Impairment & Blindness, 106(8), 466-474. DOI: https://doi.org/10.1177%2F0145482X1210600803 [ Links ]
Keszei, A., Novak, M., & Streiner, D. L. (2010). Introduction to health measurement scales. Journal of Psychosomatic Research, 68(4), 319-323. DOI: https://doi.org/10.1016/j.jpsychores.2010.01.006 [ Links ]
Matos, M. R., Matos, C. P. G., & Oliveira, C. S. (2010). Equilíbrio estático da criança com baixa visão por meio de parâmetros estabilométricos. Fisioterapia e Movimento, 23(3), 361-369. [ Links ]
Polit, D. F., & Beck, C. T. (2006). Using research in evidence-based nursing practice. Philadelphia: Lippincott Williams & Wilkins. [ Links ]
Rosa Neto, F. (2015). Manual de Avaliação Motora. Florianópolis: DIOESC. [ Links ]
Sánchez, P. A. (1994). Deficiencias visuales y psicomotricidad: teoría y práctica. Madrid: Organización Nacional de Ciegos Españoles. [ Links ]
Santos, L. C., Passos, J. E. de O. S., & Rezende, A. L. G. (2007). Os efeitos da aprendizagem psicomotora no controle das atividades de locomoção sobre obstáculos em crianças com deficiência da visão. Revista Brasileira de Educação Especial, 13(3), 365-380. DOI: https://doi.org/10.1590/S1413-65382007000300005 [ Links ]
Schmitt, B. D., & Pereira, K. (2014). Caracterização das ações motoras de crianças com baixa visão e visão normal durante o brincar: cubos com e sem estímulo luminoso ou alto contraste. Revista Brasileira de Educação Especial, 20(3), 435-448. DOI: https://doi.org/10.1590/S1413-65382014000300009 [ Links ]
Schmitt, B. D., Pereira, K. (2016). Frequência de ações motoras em crianças com baixa visão e visão normal ao explorar cubos com e sem estímulos visuais. Revista Brasileira de Educação Especial, 22(3), 399-412. DOI: https://doi.org/10.1590/S1413-65382216000300007 [ Links ]
Souza, A. C., Alexandre, N. M. C., & Guirardello, E. D. (2017). Propriedades psicométricas na avaliação de instrumentos: avaliação da confiabilidade e da validade. Epidemiologia e Serviços de Saúde, 26(3), 649-659. DOI: https://doi.org/10.5123/s1679-49742017000300022 [ Links ]
Streiner, D. L., & Norman, G. R. (2008). Health measurement scales. A practical guide to their development and use. Nova York: Oxford University Press. [ Links ]
Topor, I. (2014). Essential elements in early intervention: visual impairment and multiple disabilities. Nova York: American Foundation for the Blind Press. [ Links ]
Uysal, S. A., & Düger, T. (2011). A comparison of motor skills in Turkish children with different visual acuity. Fizyoterapi Rehabilitasyon, 22(1), 23-29. [ Links ]
World Health Organization (2013). Media centre. Visual impairment and blindness. Recuperado em 24 de agosto de 2017 de http://www.who.int/mediacentre/factsheets/fs282/en/ [ Links ]
Received: August 09, 2019; Revised: February 08, 2020; Accepted: February 22, 2020











 texto em
texto em 



