INTRODUCTION
The use of medicinal plants is based on the accumulation of information for successive generations and constituted the basis for the treatment of different diseases1. It started to be officially recognized by the World Health Organization (WHO) as of 1978, during the International Conference on Primary Health Care, by the Alma-Ata Declaration2.
In Brazil, several initiatives to include phytotherapy and other practices have been made since 1980. Concepts about alternative practices in health services were introduced at the 8th National Health Conference3. In 2006, the National Policy for Integrative and Complementary Practices (PNPIC) and the National Policy on Medicinal Plants and Herbal Medicines (PNPMF) were approved, which included phytotherapy, aiming at guaranteeing safe access and rational use of medicinal plants and herbal medicines4,5.
As part of the PNPMF, the Ministry of Health (MoH) in 2007 included herbal medicines in the list of essential medicines, aiming to stimulate and support their use in the public network and, currently, 12 of them are part of the National List of Essential Medicines (RENAME), which can be acquired through subsidy from the pharmaceutical assistance policy6.
After phytotherapy was established as a health policy and phytotherapy drugs were made available, the need for training professionals in public health care networks was evidenced, mainly due to deficiencies in undergraduate or even refreshing courses. In 80% of the medicinal plants and herbal medicine programs evaluated in Brazil, physicians who did not adhere to phytotherapy services attribute it to the fact that they do not have the knowledge, and 71% indicated training courses as a strategy to increase the adherence of prescribers7.
In 2012, the Department of Pharmaceutical Assistance and Strategic Inputs of the Science, Technology and Strategic Input Secretariat of the Ministry of Health performed the Phytotherapy Distance Learning Course for the Brazilian Unified Health System (SUS) physicians, which included 313 enrolled physicians, 191 (61%) of which finished the course8.
Recently, the MoH started the distance learning course open to health professionals, to those who work in the Family Health Strategy and Family Health Support Center teams, which has the collaboration of several institutions, such as Center for Ethnobotanical and Ethnopharmacological Studies (CEE / UNIFESP)9.
“MEDICINAL PLANTS AND PHYTOTHERAPY” COURSE IN SÃO PAULO
In 2006, the Secretariat for the Environment (SVMA) of the City Hall of São Paulo (PMSP) took the initiative to promote a pilot course on “Medicinal Plants” and to support the course, the book “Medicinal Plants” was created10. The 1st edition of the Course started in 2009, aiming at collaborating with public health policies, assisting in the implementation of actions / services related to the PNPMF, and contributing to the Phytotherapy Drugs and Medicinal Plants Program in the city of São Paulo11, regulated in 201012.
From 2009 to 2013, there were two editions of the “Medicinal Plants” course per year and, as of 2014, the course was expanded and renamed “Medicinal Plants and Phytotherapy”, starting to be held once a year13,14.
As of 2011, courses started to be held at the Open University of the Environment and Culture of Peace (UMAPAZ / SVMA), in partnership with the São Paulo Municipal Health Secretariat (SMS-SP). This partnership, stimulated by the participation of several professionals from the health network in the courses, including in municipalities close to the capital, such as Guarulhos, was a decisive factor for the initiatives to implement phytotherapy as a local policy. As developments, we mention in the SMS-SP the creation of a multiprofessional commission, preparation of Medicinal Plants notebooks, implantation of medicinal gardens with the encouragement of the Green and Healthy Environment Program (Pavs, Programa Ambientes Verdes e Saudáveis), a course for prescribers, a Memento edition with 4 herbal medicines in the network (Maytenus ilicifolia, Harpagophytum procumbens, Valeriana officinalis and Glycine max)15 and, in Guarulhos, the inclusion of 2 herbal medicines (Mikania glomerata and Glycine max)16.
Since the 1st edition, the course has been validated for the purpose of promotion and functional progression for effective career professionals at PMSP. From 2009 to 2017, 14 classes have graduated and more than 1,500 professionals from different academic backgrounds have been trained17.
In view of the relevance that the SVMA’s “Medicinal Plants and Phytotherapy” course has shown in recent years, it was decided to evaluate its contribution and impact on the phytotherapy practices of health professionals trained in the years 2014 and 2015.
METHOD
This is an exploratory, descriptive study with a qualitative and quantitative approach, approved by the Research Ethics Committees of UNIFESP with a Certificate of Ethical Appreciation Presentation (CAAE n. 62111216.6.0000.5505), by SMS-SP (CAAE 62111216.6.3001.0086) and approved by the Health Secretariat of Guarulhos. The research participants signed the Free and Informed Consent (FIC) form in compliance with the National Health Council regulations18.
For this study, the following concepts were used: Medicinal plant - plant species, cultivated or not, used for therapeutic and / or prophylactic purposes19; Vegetable drug - medicinal plant, or its parts, that contains the substances responsible for the therapeutic action, after the collection/harvesting, and stabilization, when applicable, and drying process, of its whole, shredded, crushed or pulverized form20; Phytotherapy drug - product obtained from a medicinal plant or its derivatives, except for pharmacologically active isolated substances, with prophylactic, curative or palliative purposes19. An explanatory and illustrative poster was used in the interviews in order to avoid confusion between the three concepts above.
The set comprising the concepts of medicinal plant, vegetable drug and phytotherapy drug is referred to in this work as “plant-based products” (PBP).
According to the scheme shown in Figure 1, the study was initially carried out with 300 health professionals from the city capital of São Paulo and Guarulhos who graduated from the “Medicinal Plants and Phytotherapy” course in the 2014 (150 participants) and 2015 (150 participants) editions. For the course enrollment process, the health professionals were appointed by the Primary Care Sector of the Municipal Health Secretariats involved in the project and at the time of enrollment they filled out a registration form containing several questions to assess knowledge and work in the area of medicinal plants / phytotherapy before the course, and their expectations, among others. The data obtained from this form were added to those obtained from the interview script, which will be addressed below in Phase II of this study, to expand the analysis of the participants’ knowledge before the course.
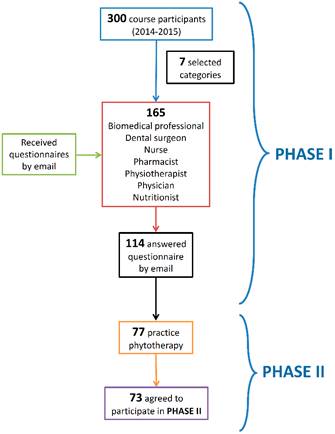
Source: Authors’ own
Figure 1 Scheme of the distribution of participants of the “Medicinal Plants and Phytotherapy” course (2014 and 2015) in Phases I and II of the study.
The inclusion criteria in the study were: obtaining passing grades in the course and academic training with attribution for recommendation and / or prescription of PBP, according to federal normative acts of each professional category. Of the total participants, 165 professionals met the criteria and were selected to participate in the study, which was divided into two phases (Figure 1).
In Phase I (quantitative study), an invitation and a questionnaire adapted from Akiyama21 were sent by email to the 165 participants who finished the course (80 from the 2014 edition and 85 from 2015), to collect sociodemographic data, information about professional training and development of activities related to phytotherapy in professional practice, with predominantly closed (yes / no) and multiple-choice questions. Data collection took place in January 2017 and the return rate comprised 114 finished and returned the questionnaires (Figure 1).
In Phase II (qualitative and quantitative study), 77 professionals (30 from the 2014 edition and 47 from 2015) who, in Phase I, reported carrying out practices related to phytotherapy, were included in the study, of which 73 accepted to participate in a semi-structured, individual, in-person interviews (Figure 1). During the qualitative study, an interview script with open questions was applied, allowing the increase in the knowledge and a deeper understanding of the investigated phenomenon22,23,24,25. This script addressed aspects of the knowledge about phytotherapy and professional performance of the participants (recommendation and prescription of PBP, knowledge of its risks, simultaneous use of synthetic drugs, adverse reactions and notification, among others); before and after the course. Therefore, answers were obtained about: “Which herbal medicines did you prescribe before the course?” And “Which herbal medicines did you start to prescribe after the course?”. The script also consisted of closed questions (yes/no) from a quantitative point of view, such as: “Did you prescribe herbal medicines before the course?” And “Did you start prescribing herbal medicines after the course?”, so that issues related to the topic could be explored by the interviewers, from a qualitative point of view. The interviews took place between March and June of 2017 and were carried out by two previously trained health professionals and not by the study main researcher, who is the creator and coordinator of the courses (L.M.M. Haraguchi), in order to avoid conflicts of interest.
The questions with a quantitative approach were analyzed through absolute frequency and percentages and by Pearson’s chi-square test (x2). McNemar’s statistical test was used to verify whether there was a significant difference in the participants’ responses before and after the course, to allow the assessment of the impact of the course on the several analyzed aspects. As for the open-ended questions, for the purposes of statistical analysis, the answers that were selected showed a citation frequency ≥10%. For the statistical tests, significant differences were considered when p≤0.05.
The qualitative data were analyzed using content analysis24,25. The data were summarized into thematic categories, allowing a reflection on the results, inferences and interpretations26.
RESULTS AND DISCUSSION
1.1 Phase I - As detailed in Figure 1, of the 300 participants who finished the course in 2014 and 2015 (150 participants per year), 165 (80 from the 2014 edition and 85 from 2015) met the inclusion criteria and were selected for the study in Phase I and received an invitation and questionnaire by e-mail. A total of 114 questionnaires were returned (Response rate of 69% - Table 1).
Table 1 Sociodemographic and training data of health professionals from the capital city of São Paulo and Guarulhos who finished the course “Medicinal Plants and Phytotherapy” in the 2014 and 2015 editions, and distribution of the response rate to the study questionnaire.
| Sociodemographic and training data | N. of sent questionnaires | N. of answered questionnaires | % | |
|---|---|---|---|---|
| Gender | Male | 18 | 11 | 61% |
| Female | 147 | 103 | 70% | |
| Total | 165 | 114 | 69% | |
| Age range | 21 to 30 years | 17 | 8 | 47% |
| 31 to 50 years | 82 | 57 | 70% | |
| 51 years or older | 66 | 49 | 74% | |
| Total | 165 | 114 | 69% | |
| Professional category | Biomedical professional | 2 | 2 | 100% |
| Physiotherapist | 3 | 2 | 67% | |
| Nutritionist | 20 | 14 | 70% | |
| Physician | 27 | 19 | 70% | |
| Nurse | 33 | 19 | 58% | |
| Dental surgeon | 30 | 20 | 67% | |
| Pharmacist | 50 | 38 | 76% | |
| Total | 165 | 114 | 69% | |
Source: Authors’ own
Of the 114 effective study participants (Table 2), 77 (68%) reported performing practices related to phytotherapy. The proportion of participants who practiced phytotherapy was homogeneous among the professional categories.
Table 2 Practices related to phytotherapy carried out by the health professionals from the city capital of São Saulo and Guarulhos who finished the course “Medicinal Plants and Phytotherapy” in the 2014 and 2015 editions.
| Professional category | Practice | Do not practice | Total | p-value* | ||
|---|---|---|---|---|---|---|
| N | % | N | % | N | ||
| Physician | 16 | 84 | 3 | 16 | 19 | |
| Nurse | 14 | 74 | 5 | 26 | 19 | |
| Dental surgeon | 13 | 65 | 7 | 35 | 20 | |
| Nutritionist | 9 | 64 | 5 | 36 | 14 | |
| Pharmacist | 23 | 61 | 15 | 39 | 38 | |
| Biomedical professional | 1 | 50 | 1 | 50 | 2 | |
| Physiotherapist | 1 | 50 | 1 | 50 | 2 | |
| Total | 77 | 68 | 37 | 32 | 114 | 0.384 |
* Pearson’s Chi-square Test (x2). Source: Authors’ own
The results highlight the fact that the practice of phytotherapy occurs regardless of the professional category.
The study also assessed whether phytotherapy practice is more related to a Specialization degree (Postgraduate lato sensu studies): 9 of the 9 professionals with a specialization in Phytotherapy (100% practice phytotherapy); 6 out of 6 with specialization in Pediatrics (100%); 8 of 9 with a specialization in Homeopathy (89%); 11 of 15 with a specialization in Collective Health (73%); 19 of 29 with a specialization in Public Health (66%); 4 of 7 with a specialization in General Practice (57%); 5 of 9 in Clinical Pharmacy (56%) and 4 of 9 in Acupuncture (44%).
Nagai and Queiroz27 found similar situations, since, among the causes of the successful implementation of complementary and alternative practices in the public health network, the support of health professionals was emphasized, according to their health viewpoints.
The high prevalence of practice among professionals with specialization in areas related to integrative and complementary practices (ICPs) reflected what was expected for Phytotherapy and Homeopathy in the present study; however, the result observed among the acupuncture specialists (4 of 9 professionals practice phytotherapy), an area in which plants are present, whether to be used in moxibustion or in the prescription of species of Traditional Chinese Medicine, were noteworthy.
One of the questions of the questionnaire was open and allowed comments about the course. Of the 114 participants, 96 (84%) made 271 different comments, 221 of them (82%) praising the course, 44 (16%) suggestions and 6 of them (2%) criticisms. While the majority positively evaluated the course, the qualifications of the teachers, the syllabus and the approach, the criticisms focused on the excessive number of participants, the small inclusion of clinical cases, the dissemination restricted to the public health care network and the lack of topics aimed at each profession.
1.2 Phase II - Of the 114 professionals who participated in Phase I, 73 were included in Phase II since, among the 77 participants who reported performing practices related to phytotherapy, 4 did not accept to participate in the interviews (Figure 1).
The results of the dichotomous questions (yes/no) of the interview script related to phytotherapy practices performed before and after the course are shown in Table 3. The evaluation of the impact of the training course disclosed a significant improvement (p≤0.001) regarding all aspects of phytotherapy care - PBP recommendation and prescription; knowledge of the risks and questions about the simultaneous use of PBP and synthetic drugs - except for the knowledge and notification of adverse reactions to PBP (Table 3).
Table 3 Practices related to phytotherapy care performed before and after the course by the 73 professionals who finished the course “Medicinal Plants and Phytotherapy” in the 2014 and 2015 editions, selected for Phase II of this study.
| Topic | YES | Yes/Yes | No/No | No/Yes | Yes/No | Difference % | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | N | N | N | N | |||||
| N | % | N | % | |||||||
| Recommendation of medicinal plants | 37 | 51 | 67 | 92 | 37 | 6 | 30 | 0 | 41 | <0.001 |
| Recommendation of vegetable drugs | 33 | 45 | 64 | 88 | 33 | 9 | 31 | 0 | 43 | <0.001 |
| Prescription of herbal medicines | 25 | 34 | 60 | 82 | 24 | 12 | 36 | 1 | 48 | <0.001 |
| Questions about the simultaneous use of synthetic drugs (N=671) | 31 | 46 | 61 | 91 | 31 | 6 | 30 | 0 | 45 | <0.001 |
| Knowledge of risks | 53 | 73 | 72 | 99 | 53 | 1 | 19 | 0 | 26 | <0.001 |
| Recognition of adverse reactions | 7 | 10 | 7 | 10 | 1 | 60 | 6 | 6 | 00 | NS |
| Notification of adverse reactions | 0 | 0 | 0 | 0 | 0 | 73 | 0 | 0 | - | NP |
McNemar Statistical Test - significant difference (p≤0.05) 1Participants who provided direct care to the patient, performing anamnesis NS: not significant NP: not performed Source: Authors’ own
Table 3 shows that, before the course, there was a greater number of professionals who recommended medicinal plants in comparison to those who prescribed herbal medicines (51% and 34%, respectively), perhaps reflecting a mistaken concept, that the use of “teas” is inherently safer than industrialized products. After the training, there was a significant increase (p <0.001) both in the number of professionals who recommended medicinal plants/vegetable drugs and those who prescribed herbal medicines (92% and 82%). This picture was also found by Araújo28, with a predominance of the recommendation of medicinal plants (65%) in relation to the prescription of herbal medicines (27.5%). Curiously, one could expect the opposite, since industrialized herbal medicines, when submitted to the regulatory organ’s assessment, are marketed with proven evidence, defined doses and package inserts.
Table 3 also shows there is a significant increase in the number of herbal medicine prescribers (from 25 to 60), suggesting a positive impact of the course regarding this aspect, which had as a facilitators for this change the presentation of evidence-based herbal medicine, as the dissemination of studies on scientific proof of the effects of PBP is necessary for the institutionalization of phytotherapy in primary care29, just as it should be for any other type of therapy and at any level of health care.
In fact, 95% of Phase II participants (69 professionals) replied that the course contributed to the professional practice in their area of care and that they felt more prepared to advise, recommend, and prescribe PBP (Graphic 1); the remaining four participants (5%) justified acting in areas other than phytotherapy. The comments among those who responded positively were categorized and grouped into topics, considering at least 2 citations by different professionals (Graphic 1). This result corroborates the study that characterized the inclusion of phytotherapy into Primary Health Care (PHC) in our country30, which, based on the analysis of 53 studies, points to the continuing and permanent education of health teams as a stimulating factor for the prescription of herbal medicines and medicinal plants.
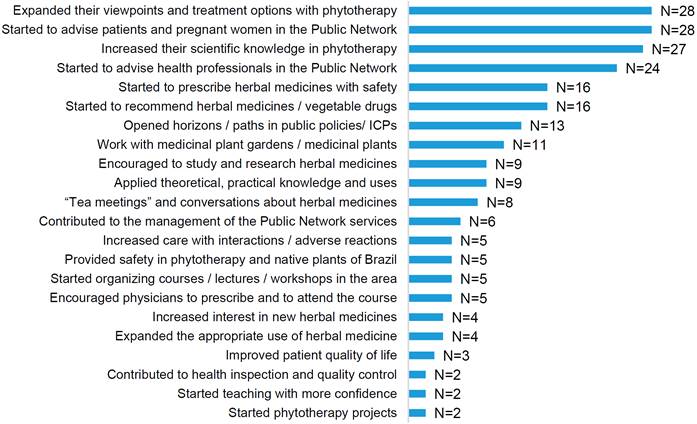
Source: Authors’ own
Graphic 1 Distribution of comments on the contribution of the course to professional practice, quoted by the 69 health professionals (Phase II) participating in the course “Medicinal Plants and Phytotherapy” (2014 and 2015).
The comments below reflect the main results demonstrated in the study:
- “After the course I started to recommend, indicate and prescribe herbal medicine, I am no longer against it.” (Physician);
- “When the patients say they use medicinal plants, I don’t have that inflexible attitude anymore. I advise and teach patients how to use them correctly.” (Physician);
- “I did not have a lot of information and we have popular beliefs; the course offers a technical and scientific viewpoint, it provided a theoretical basis.” (Dental Surgeon);
- “This course gave me a technical-scientific basis, in addition to indicating excellent literature and scientific works” (Nurse);
- “After the course, we (a physician, a nutritionist and a pharmacist) founded a group about plants with patients and professionals and we have monthly meetings” (Pharmacist);
- “In my professional practice, I had a viewpoint aimed at medication and disease, and the human being is more than that. I started to have a more holistic view of the human being and health.” (Pharmacist);
- “I learned a lot, the course allowed me to have a new perspective, I started to apply, use, indicate and I became interested in phytotherapy after the course.” (Dental Surgeon).
After the course (Table 3), a significant increase was observed in the number of professionals that knew that PBP can bring health risks (from 73% to 99%). In addition to addressing PBP efficacy/effectiveness, the course considered aspects related to safety regarding the use of these products, seeking to deconstruct the myth that the use of medicinal plants is risk-free, a belief that is part of the population’s cultural background - “what comes from the earth cannot harm you”31, and it is also found among health professionals, as demonstrated in this study, especially before the training, possibly due to lack of knowledge on the subject.
There was a significant increase (from 46% to 91%) in the number of professionals who asked the user about the concomitant use of PBP and synthetic drugs, although 6 professionals remained unaware of the importance of this evaluation (Table 3). Asking about the use of medicinal plants and related products is one of the topics considered essential during the interview to obtain the patient’s medication history32 being recommended during treatment with any type of medication, due to the possibility of interaction between them. However, many professionals do not ask this question, possibly because they are unaware of the risks, the types of possible interactions, the consequences and/or how to proceed in cases of interaction between medications and medicinal plants. Studies have shown little familiarity of health professionals regarding interactions between plants or these with medications33,34.
In the present study, during the interviews, two reports were made of the detection of interactions between plants and medications, involving the interaction between sertraline and Hypericum perforatum (St. John’s wort), generating exacerbation of serotonergic effects; and between Daflon® and Ginkgo biloba, causing coagulation alterations, which were solved in clinical practice based on the knowledge obtained in the course, according to a report by a former student:
“Hypericum perforatum interacted with sertraline and caused serotoninergic syndrome in a hospital patient. I was called to treat the case, took the course book and showed it to the neurologist, who discontinued the use and solved the problem. I felt good, because I was called and became a technical reference in this area after taking this phytotherapy course; showing that the herbal medicine (Hypericum) was a real medication and that it had interaction and deserved all the care” (Physician).
Regarding the professionals who were aware of or followed cases of adverse reactions with PBP in clinical practice, Table 3 shows that there was no difference in the total number (7 professionals before and 7 after the course). However, it was observed that for 6 professionals this only occurred after the training (period of 1 to 2 years, that is, between the course and the interview), whereas 6 professionals reported that they had knowledge of or followed adverse reaction cases before the course, that is, during their professional life before the training (period that varied between years and decades). Thus, a more in-depth analysis of the data suggests that, for professionals who recognized adverse reactions to PBP, the training may have had an impact on the level of care, collection and/or increased importance of patient information on possible adverse effects to the used treatment. However, among the 66 professionals who did not report cases of adverse reactions observed before the training, 60 continued without a case to report after the training.
Several factors can contribute to the lack of case identification by the health professional, such as problems in monitoring the results of the proposed treatment, failure to suspect adverse reactions to medications, the professional’s difficulty in accepting that the prescribed medication may have caused negative results, lack of information about the risks of the recommended treatment, as well as lack of communication from the patient, to the professional, about a possible undesirable effect. It is also possible that patients did not have any undesirable effects during this period, due to the established safety of the medicinal plants used in the treatment.
On the other hand, an improved reporting of adverse reactions after training was observed. The case reports that occurred before the training involved general malaise with the use of a folk medicine prepared with “folhas de chuchu” (chayote leaves), allergy to “aroeira” (Brazilian pepper tree), skin irritation caused by “comigo-ninguém-pode” (Dumb cane) and “coroa-de-cristo” (Christ thorn) and other unspecified cases involving “porangaba” (Cordia ecalyculata Vell.), “erva-de-santa-maria” (wormseed) and “urucum” (annatto); therefore, they are generic reports, without details, typical of a superficial evaluation of the cases, many of which are skin reactions, easy to identify. After training, cases of changes in blood pressure during the use of hibiscus, changes in liver enzymes with the use of Tribulus terrestris an unspecified reaction with annatto, unspecified skin reactions with unknown species were reported. Although still incomplete, they show an increase in knowledge on the topic, which improves the detection and characterization of adverse reactions. Such differences can be credited, at least in part, to the awareness and training of professionals on the topic.
However, although some participants recognized adverse reactions during the use of PBP, none of the professionals had the initiative to carry out the notification, both before and after the course. This result, associated with the information that herbal medicines represent only 0.4% of the total notifications of adverse reactions to ANVISA’s Pharmacovigilance database35, suggests the need to promote health professionals’ awareness more intensively about the importance of adverse reaction notifications, as well as the procedure to be performed, to increase the knowledge of the risks and, consequently, to allow the identification and dissemination of information on how to manage the adverse reactions, making it possible to prevent them or attenuate their consequences, thus promoting the safe use of medicinal plants and herbal medicines.
Table 4 shows the evaluation of the differences before and after the course in relation to the recommended / prescribed PBP.
Regarding medicinal plants and vegetable drugs, there was a significant increase, after the course, in the number of professionals who recommended / prescribed chamomile, espinheira-santa, lemon balm and aloe, among others.
Table 4 Impact of the phytotherapy training on the recommendation / prescription of medicinal plants, vegetable drugs and herbal medicines, by the 73 professionals who finished the course “Medicinal Plants and Herbal Medicines” in the 2014 and 2015 editions, selected for Phase II of this study.
| Medicinal plants 1 | YES | Yes/Yes | No/No | No/Yes | Yes/No | Difference % | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Before | After | N | N | N | N | |||||
| N | % | N | % | |||||||
| Chamomile | 12 | 16.4 | 28 | 38.4 | 12 | 45 | 16 | 0 | 21.9 | <0.001 |
| Espinheira-santa | 1 | 1.4 | 15 | 20.8 | 1 | 57 | 14 | 0 | 19.4 | <0.001 |
| Aloe | 3 | 4.1 | 12 | 16.4 | 3 | 61 | 9 | 0 | 12.3 | <0.001 |
| Lemon balm | 15 | 20.5 | 30 | 41.1 | 15 | 43 | 15 | 0 | 20.5 | <0.001 |
| Boldo | 6 | 8.2 | 14 | 19.2 | 6 | 59 | 8 | 0 | 11.0 | 0.008 |
| Mint | 9 | 12.3 | 16 | 21.9 | 9 | 57 | 7 | 0 | 9.6 | 0.016 |
| Huaco | 8 | 11.0 | 13 | 17.8 | 8 | 60 | 5 | 0 | 6.9 | NS |
| Vegetable drugs1 | ||||||||||
| Chamomile | 15 | 20.6 | 33 | 45.2 | 15 | 40 | 18 | 0 | 24.6 | <0.001 |
| Espinheira-santa | 1 | 1.4 | 18 | 24.7 | 1 | 55 | 17 | 0 | 23.3 | <0.001 |
| Lemon balm | 7 | 9.6 | 21 | 28.8 | 7 | 52 | 14 | 0 | 19.2 | <0.001 |
| Fennel | 8 | 11.0 | 16 | 22.0 | 8 | 57 | 8 | 0 | 11.0 | 0.008 |
| Mint | 3 | 4.1 | 11 | 15.1 | 3 | 62 | 8 | 0 | 11.0 | 0.008 |
| Boldo | 4 | 5.5 | 10 | 13.7 | 4 | 63 | 6 | 0 | 8.2 | 0.031 |
| Horsetail | 2 | 2.7 | 9 | 12.3 | 2 | 64 | 7 | 0 | 9.6 | 0.016 |
| Herbal medicines 2 | ||||||||||
| Valeriana - Valeriana officinalis | 2 | 2,7 | 35 | 48,0 | 2 | 38 | 33 | 0 | 45,2 | <0,001 |
| Espinheira-santa - Maytenus ilicifolia | 3 | 4,1 | 32 | 43,8 | 3 | 41 | 29 | 0 | 39,7 | <0,001 |
| Devil’s claw - Harpagophytum procumbens | 1 | 1,4 | 20 | 27,4 | 1 | 53 | 19 | 0 | 26,0 | <0,001 |
| Soy isoflavone - Glycine max | 1 | 1,4 | 14 | 19,2 | 1 | 59 | 13 | 0 | 17,8 | <0,001 |
| Passionfruit - Passiflora incarnata | 5 | 6.9 | 14 | 19.2 | 5 | 59 | 9 | 0 | 12.3 | 0.004 |
| Chamomile - Matricaria chamomilla | 3 | 4.1 | 10 | 13.7 | 3 | 63 | 7 | 0 | 9.6 | 0.015 |
| Huaco - Mikania glomerata | 1 | 1.4 | 8 | 11.0 | 1 | 65 | 7 | 0 | 9.6 | 0.015 |
| Ginkgo - Ginkgo biloba | 3 | 4.1 | 7 | 9.7 | 3 | 65 | 4 | 0 | 5.6 | NS |
McNemar Statistical Test - significant difference (p≤0.05) 1Unverified species; 2Species according to the product package inserts. NS: nonsignificant Source: Authors’ own
These results are probably related to highlighted plants during the course classes, as occurred with chamomile and the European lemon balm (Melissa officinalis), species with good scientific evidence and generally addressed in different therapeutic modules. In the case of espinheira-santa (Maytenus ilicifolia), its importance is due to the fact that it is a good therapeutic option to the generalized consumption of omeprazole in the public network36.
Chamomile was among the most frequently used medicinal plants by health professionals in studies carried out in Brazil29,34, as well as the espinheira-santa29.
As for herbal medicines, the highlights involved products based on valeriana, espinheira-santa, devil’s claw and soy isoflavone (Table 4). The significant increase in the prescription of these herbal medicines stems from good clinical evidence and coincides with the implementation of the herbal medicine program at SMS-SP15, which standardized and made available these four products in 2014 and, therefore, were addressed during the course classes in 2014 and 2015.
There was no significant difference in the number of professionals who prescribed huaco as a medicinal plant and ginkgo as a herbal medicine, before and after the course (Table 4). In the case of huaco, its clinical evidence is small, although the species is present in herbal medicine programs in the country. In relation to ginkgo, the species is present in widely used industrialized herbal medicines; on the other hand, it is also known for blood clotting alterations37, which requires caution in its prescription.
Differences were assessed before and after the course in relation to therapeutic indications and PBP uses. Regarding therapeutic indications, the higher number of professionals who recommended / prescribed PBP for dyspepsia/gastritis and anxiety/insomnia was already highlighted, and there was a significant increase after the course (from 26 to 52% and from 25 to 49%, respectively) and also herbal medicines (from 8 to 43% and from 7 to 51%), justifying the recommendation and prescription data related to espinheira-santa (gastroprotective), valeriana, chamomile and lemon balm (central nervous system depressants) (Table 4). It should be noted that, despite the emphasis seen in the digestive system pathologies module on the differences between dyspepsia and gastritis that require opposing treatments, according to the Rome III Consensus [38], in practice the widespread use of espinheira-santa is confirmed for both conditions, which is not appropriate.
The majority of indications for gastritis / dyspepsia and anxiety / insomnia coincide with the indications for the most frequently currently consumed synthetic drugs in the municipal health network of São Paulo, demonstrating the potential of PBP as an alternative to synthetic drugs.
In addition to dyspepsia / gastritis and anxiety / insomnia, there was a significant increase in the number of professionals prescribing herbal medicines for rheumatic conditions (from 1 to 29%) and menopause (from 3 to 22%), certainly related to devil’s claw and soy isoflavone-based products, detailed during the course and available on the municipal health network.
Similar results were found in other studies in which the most frequently mentioned therapeutic indications were tranquilizers, stomach problems (dyspepsia), anti-inflammatory and sleep-inducing medicines29, as well as those for the digestive system, sedatives and skin problems34.
Regarding the forms of use of PBP, before the course there was a predominance of professionals who indicated infusions and decoctions, both for medicinal plants and vegetable drugs. After the course, this number increased significantly (from 49 to 84%), showing the importance of this form of use in herbal medicine and reinforcing the data obtained by Valverde et al.39 regarding the predominance of the use of teas by infusion (53%).
After the training, there was a significant change in the search for academic knowledge, since there was a significant increase in the number of professionals who felt encouraged to take courses related to herbal medicine (from 29% to 85%), especially post-graduate lato sensu courses in phytotherapy (from 7% to 22%). This result shows the importance of training in the theoretical-practical preparation required to provide quality care and as a stimulus to continuing education in phytotherapy. Studies point out the importance of training and that the lack of knowledge, qualification and training of health professionals in ICPs, medicinal plants / phytotherapy are negative aspects that prevent the inclusion of phytotherapy in PHC7,40,41,42.
CONCLUSIONS
The results suggest that the training provided by the course “Medicinal Plants and Phytotherapy” has had a positive impact on the practice of phytotherapy carried out by professionals from the municipal public health system in São Paulo and Guarulhos, regarding several aspects, contributing to the expansion and improvement of phytotherapy care to patients, in addition to stimulating the professionals to improve their knowledge on the topic.
The course showed a significant increase in the use of plant-based products such as chamomile, espinheira-santa and valeriana. For 95% of the participants, the course contributed to the expansion of phytotherapy practice. The course did not change the professionals’ practice regarding the notification of adverse reactions. The study showed the importance of including the area of phytotherapy and medicinal plants in the curriculum of undergraduate courses in the health area. This work contributed to support training activities as an important instrument for the consolidation of public policies.











 texto em
texto em 



