INTRODUCTION
Common Mental Disorders (CMD) correspond to clinical conditions in which the individual has symptoms of anxiety, depression, sadness, fatigue, insomnia, stress, irritability, and somatic complaints, such as anorexia, dyspnea, and headache, among others1)-(3. However, these manifestations do not meet enough criteria for a formal psychological diagnosis of depression and / or anxiety according to the DSM-V (Diagnostic and Statistical Manual of Mental Disorders - 5th edition) and ICD-11 (International Classification of Diseases - 11th revision) classifications4),(5, although they show an intensity and frequency capable of resulting in psychological distress for individuals, interfering in their daily activities, their interpersonal relationships and quality of life1),(2),(6),(7.
It is estimated that CMDs affect 9% to 12% of the world’s population and 12% to 15% of the Brazilian population in all age groups8. According to the World Health Organization (WHO), this number has been increasing worldwide, especially in low-income countries, in females, the poorest and the unemployed, precisely those in which the symptoms of anxiety and depression are more frequent9)-(11. In Brazil, the prevalence of CMDs, according to several authors, ranges from 19.7% to 43.7%, which represents a significant portion of the population that may require specialized care12),(13.
Among the different social groups, university students are more vulnerable to the development of anxiety and depression disorders, and there have been studies that used different instruments, such as the Self-Reporting Questionnaire (SRQ-20)14, the Beck Anxiety Inventory (BAI)15, and the Beck Depression Inventory (BDI)16, which demonstrated its high prevalence, especially among medical students in several continents16),(17. In economically developing countries, such as Egypt, a study carried out with 700 medical students in the year 2017 reported a high prevalence of anxiety, of 73%, and a prevalence of depression of 65%18. In Turkey, they found a prevalence rate of 35.8% for symptoms of medium and moderate anxiety and 30.5% for medium and moderate depression and 8.5% for severe depression19.
In turn, in Brazil in 2015, studies carried out with medical students from the state of Santa Catarina disclosed a prevalence of 35.5% and 32.8%, respectively for anxiety and depression21. At Faculdade Pernambucana de Saúde (FPS), in 2014, the prevalence was 19.7% for anxiety and 5.6% for depression21.
Considering this scenario of high CMD frequency in university students, the aim of this study was to estimate the prevalence rate and factors associated with symptoms of anxiety and depression in medical students in a capital city in northeastern Brazil in 2018.
METHODS
This is a prevalence study, with a probabilistic sample of 1,339 students who regularly attended all 12 semesters of the medical course in January 2018 and who signed the Free and Informed Consent Form / Term of Assent. For the sample size calculation, we considered as parameters an expected mean prevalence of anxiety and depression symptoms in university students of 35%20),(22),(23, an acceptable alpha error of 5% (α = 5%), an effect of design of 1.5 and a 95% confidence level. The sample size was estimated at 417 students, which after adding 10% for losses and refusals, totaled 457, divided proportionately, resulting in an average of 35 students per semester, which were selected by simple random drawing.
Data were collected by applying the following instruments: a) a structured questionnaire to record social, demographic, economic and behavioral information; b) Beck Anxiety Inventory (BAI) developed by Beck et al. (1988)15 and translated into Brazilian Portuguese and validated in Brazil in university students by Quintão et al. (2012)24 and c) Beck Depression Inventory (BDI) also developed by Beck et al. (1961)16 and validated in the Brazilian Portuguese language, in Brazil, by Gorenstein and Andrade (1996)25 and Gomes-Oliveira (2012)26. According to the cutoff points established by BAI, a score <10 was considered as absence or symptoms of minimal anxiety; 11-19, mild; 20-30, moderate; and 30-63 points as severe anxiety, whereas in the BDI for symptoms of depression, a score <10 was considered as absent or minimal; 10-18, mild; 19-29, moderate; and 30-63 points, as severe depression. For this study, a score >10 was considered as the presence of anxiety and depression symptoms.
Descriptive analyses were carried out by distributing the absolute (n) and relative (%) frequencies of the strata of the variables of interest. To check for possible differences between anxiety and depression symptoms and social, economic and behavioral variables, Pearson’s chi-square test (χ2) was used. The prevalence rates (total and by level of severity) and the crude and adjusted (Adj) prevalence ratio (PR) were used as a measure of association. The Kruskal-Wallis test was used to verify the difference between the prevalence rates, considering p <0.05 as statistical significance.
The variables that showed a crude PR with p <0.20 were incorporated into the multivariate analysis using the robust Poisson regression model, to determine the Adj PR. The data were processed and analyzed using the SPSS software, version 22 and STATA version 15.1. The study project was approved by the EBMSP Research Ethics Committee, under N. 2,519,431 on February 28, 2018 and N. 2,572,959 on April 1, 2018.
RESULTS
Of the 458 medical students (34.2% of the total) included in the study, 62.7% were females and 60.0% were aged <22 years old. The median age for both genders was 22.0 years. A total of 92.6% of the students self-declared as heterosexual, 56.7% of white ethnicity/ skin color, 60.3% had a stable boyfriend/girlfriend and 48.1% were catholics. Regarding the monthly family income, 50.1% reported their income as being <R$ 8,000.00. Students from the state where the medical school was located were 94.3%, with the vast majority, 61.3%, from the capital city. A total of 81.1% lived with family members (Table 1). Of the total number of students in the sample, 11.1% were in the first and tenth semesters of the medical course.
Table 1 Prevalence of anxiety and depression symptoms in medical students according to demographic, social, economic and behavioral variables. Salvador BA. 2018.
| Variable | Anxiety | Depression | ||||||||
| Yes | No | Yes | No | |||||||
| n | % | n | % | n | % | n | % | |||
| Gender | ||||||||||
| Female | 107 | 37.3 | 180 | 62.7 | 0.000* | 123 | 42.9 | 164 | 57.1 | 0.000* |
| Male | 34 | 19.9 | 137 | 80.1 | 42 | 24.6 | 129 | 75.4 | ||
| Age (years) | ||||||||||
| <22 | 97 | 35.4 | 178 | 64.6 | 0.011* | 100 | 36.5 | 174 | 63.5 | 0.798 |
| >22 | 44 | 24.0 | 139 | 76.0 | 65 | 35.3 | 118 | 64.7 | ||
| Sexual orientation | ||||||||||
| Homo/bisexual | 20 | 60.6 | 13 | 39.4 | 0.000* | 21 | 63.6 | 12 | 36.4 | 0.001* |
| Heterosexual | 121 | 28.5 | 303 | 71.5 | 144 | 34.0 | 280 | 66.0 | ||
| Ethnicity/skin color | ||||||||||
| Others | 58 | 29.4 | 139 | 70.6 | 0.592 | 82 | 41.6 | 115 | 58.4 | 0.030* |
| White | 82 | 31.8 | 176 | 68.2 | 82 | 31.8 | 176 | 68.2 | ||
| Affective status | ||||||||||
| With stable partner | 78 | 28.4 | 197 | 71.6 | 0.182 | 96 | 34.9 | 179 | 65.1 | 0.533 |
| No stable partner | 62 | 34.3 | 119 | 65.7 | 68 | 37.8 | 112 | 62.2 | ||
| Religion | ||||||||||
| Catholic | 62 | 28.3 | 157 | 71.7 | 0.274 | 70 | 32.0 | 149 | 68.0 | 0.081 |
| Others | 78 | 33.1 | 158 | 66.9 | 94 | 39.8 | 142 | 60.2 | ||
| Family income (R$) | ||||||||||
| <12,000,00 | 60 | 34.1 | 116 | 65.9 | 0.111 | 74 | 42.0 | 102 | 58.0 | 0.016* |
| >12,000,00 | 46 | 26.3 | 129 | 73.7 | 52 | 29.7 | 123 | 70.3 | ||
| Origin | ||||||||||
| Other states | 54 | 30.5 | 123 | 69.5 | 0.963 | 67 | 37.9 | 110 | 62.1 | 0.486 |
| Salvador | 86 | 30.7 | 194 | 69.3 | 97 | 34.6 | 183 | 65.4 | ||
| Lives with | ||||||||||
| Others | 25 | 29.1 | 61 | 70.9 | 0.680 | 41 | 47.7 | 45 | 52.3 | 0.012* |
| Family members | 116 | 31.4 | 254 | 68.6 | 123 | 33.2 | 247 | 66.8 | ||
*statistically significant
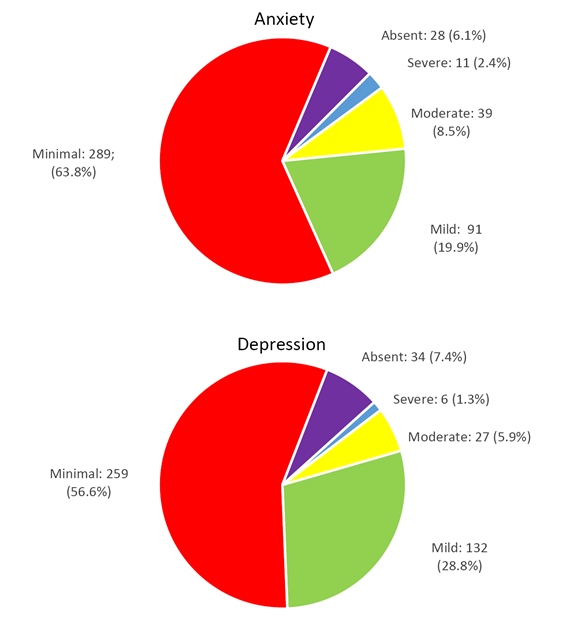
The prevalence of anxiety symptoms was 30.8%, ranging from mild, in 91 (19.9%), to moderate, in 39 (8.5%) and severe in 11 (2.4%) students. Minimal symptoms were identified in 289 (63.1%) and absent in 28 (6.1%) students. The prevalence of depression was 36.0%, ranging from mild, in 132 (28.8%), moderate, in 27 (5.9%) and severe, in 6 (1.3%) students. Symptoms were minimal in 259 (56.6%) and absent in 34 (7.4%) students (Chart 1).
The crude PR of the association of anxiety symptoms and female gender, age <22 years and homo / bisexual sexual orientation, as well as the crude PR of the association of depression symptoms and female gender, homo / bisexual sexual orientation, other ethnicity / skin color (black/brown), family income (<R$ 8,000.00) and living with others (colleagues/friend, hotel/boarding house / off-campus student residence) and alone showed a p value <0.005. In the robust Poisson model, the adjusted PR for anxiety symptoms retained a statistically significant association for gender (Adj. PR = 1.31; 95%CI [1.17-1.47]), age (Adj PR = 1.15; 95%CI [1.02-1.29]) and sexual orientation (Adj. PR = 1.90; 95%CI [1.26-2.86]) (Table 2). The adjusted PR for depression symptoms remained statistically significant for gender (Adj. PR = 1.36; 95%CI [1.20-1.55]), ethnicity / skin color (Adj. PR = 1.96; 95%CI [ 1.29-3.04]) and sexual orientation (Adj PR = 1.19; 95%CI [1.03-1.36]) (Table 3). The prevalence rate of symptoms of anxiety and depression between the basic, intermediate and internship cycles did not show a statistically significant difference, respectively, p = 0.101 and p = 0.601.
Table 2 Prevalence rate, prevalence ratio and crude and adjusted confidence interval for anxiety symptoms in medical students according to demographic, social, economic and behavioral variables. Salvador, Bahia. 2018.
| Variable | crude Odds Ratio | Confidence Interval | adjusted Odds Ratio | Confidence Interval |
| Gender: Female | 2.39 | 1.53 - 3.74 | 2.99 | 1.76 - 5.10 |
| Age: <22 years | 1.72 | 1.13 - 2.62 | 1.74 | 1.06 - 2.85 |
| Sexual Orientation: homo/bisexual | 3.85 | 1.86 - 7.99 | 3.94 | 1.74 - 8.91 |
| Affective status | 0.76 | 0.51 - 1.14 | - | - |
| Family income | 1.45 | 0.92 - 2.29 | - | - |
Table 3 Prevalence rate, prevalence ratio and crude and adjusted confidence interval for depression symptoms in medical students according to demographic, social, economic and behavioral variables. Salvador, Bahia. 2018.
| Variable | crude Odds Ratio | Confidence Interval | adjusted Odds Ratio | Confidence Interval |
| Gender: female | 2.30 | 1.51 - 3.50 | 2.86 | 1.82 - 4.51 |
| Sexual Orientation: homo/bisexual | 3.40 | 1.63 - 7.11 | 5.08 | 2.30 - 11.22 |
| Ethnicity/skin color: white | 1.53 | 1.04 - 2.25 | 1.58 | 1.05 - 2.37 |
| Religion | 0.71 | 0.48 - 1.04 | - | - |
| Family income | 1.72 | 1.10 - 2.67 | - | - |
| Lives with: family members | 1.83 | 1.14 - 2.94 | 1.94 | 1.17 - 3.21 |
DISCUSSION
The prevalence of anxiety symptoms among medical students observed in the present study (30.8%) was lower than those found by some other authors, which varied between 33.8% and 41.4%, according to Ribeiro et al. (2020)27, Moutinho et al. (2017)28, Tabalipa et al. (2015)20, Ediz et al (2017)19 and Costa et al. (2020)23. However, these same authors indicated a prevalence of symptoms of depression between 8.2% and 34.6%, therefore, lower than that of the present investigation (36.0%). It has been established that symptoms of anxiety and depression are present in the daily lives of millions of individuals worldwide, affecting both their physical and mental health, especially university students and those in the health care field.
The disagreements regarding the prevalence rates found in the literature may have occurred due to regional and cultural differences among the student population, the used methodologies and types of questionnaires used to collect the data. However, it is a consensus that the medical course is seen as one of the most difficult courses that requires the students to concentrate their efforts on dedication to the studies and that there is high competitiveness among students29. The medical student’s academic trajectory implies a long and arduous daily journey of activities, which implies in exhausting commuting that occupy even their time for social activities, leisure and even sleep hours30),(31. Another extremely important factor is the contact with the patient’s suffering, pain and even death, events that also cause tension and stress for medical students. This entire situation of physical and emotional exhaustion makes it difficult to take care of one’s own health, whether due to the students’ lack of time or negligence by the students and the school, increasing the risk of anxiety / depression symptoms and the development of burnout syndrome32),(33.
The higher prevalence of anxiety and depression in female students was similar to that found in other studies20),(21),(34, which is consistent with the Mental Health Information, according to which anxiety disorders were present in 23.4% of female individuals and in 14.3% of males35, as well as with the WHO statement, which states that worldwide, depression is more prevalent in women (5.1%) than in men (3.6%)1. Such differences, according to the WHO, are a direct consequence of gender violence, socioeconomic disadvantage, income inequality, low or subordinate social status, social demands and responsibility for the care of other individuals, such as their offspring36. Other factors may also explain, in part, this higher prevalence, such as hormonal influences, considering that testosterone can have protective benefits against anxiety and depression37.
Individuals with homo/bisexual sexual orientation showed a higher prevalence of anxiety and depression symptoms when compared with heterosexuals also associated with these outcomes. Anguish, denial, doubt and even rejection, sometimes from the family itself are problems faced by this group of individuals, since the discovery and acceptance of their sexual orientation. Therefore, there is an increase in feelings of insecurity and psychosocial problems and a reduction in self-esteem, resulting in greater vulnerability to psychosocial problems such as drug use, depression and suicide attempts38),(39. Similarly, a higher prevalence of depression symptoms was verified in students who declared themselves to be of non-white ethnicity/skin color (brown and black). This corroborates what was observed in a study with university students in the city of Rio de Janeiro40. Studies indicate that historical factors such as the lack of opportunities, both educational and socioeconomic, in addition to the stress associated with social roles and experiences such as racism and discrimination are considered important for the higher prevalence among black individuals than in white ones41),(42.
The findings by Tabalipa et al. (2015)20, Baldassin et al (2006)43 and Bastos et al. (2016)40, of a higher frequency of anxiety symptoms in students from the first to the third years of medical school, precisely the younger ones, was similar to those of our study, explained by the better adaptation of the student to the course and the strengthening of interpersonal relationships with classmates, forming groups that share similar activities, such as study, leisure, travel, etc.
Although no association was found between symptoms of anxiety and depression and living with family members, support from one’s parents is a source of strength for medical students to face difficulties during their studies and, at the same time, it also strengthens their self-confidence17),(33),(44.
Consistent with the literature, anxiety and depression symptoms were more frequent among students in the 3rd, 5th and 9th semesters of medical school. Considering the course cycles, the basic one showed a higher prevalence than the other cycles, similar to that found by Costa et al. (2020)23. Upon entering the university, students are faced with an environment that is completely different from what they had been experiencing in the previous years of study45),(46. In the first years of college, during the period of the basic course, there is an urgent need for integration with the new colleagues and adaptation to the new teaching methodology, with an excessive amount of theoretical content, tests, seminars and other pedagogical demands, which end up stressing the students, resulting in the exacerbation of anxiety and depression symptoms44. This new teaching modality requires the student to develop cognitive and emotional capacity capable of meeting this new demand, which has a great impact on quality of life, with scarcity of free time and fatigue being mentioned by the students as the main factors that affect their quality of life47),(48. In this study, the prevalence rates, both of anxiety and depression, also showed high values in the last cycle, the internship. It is believed that a closer contact with patients, often incorporating their worries, fears, anxieties and depression, makes the students into an extension of these patients, which, added to the expectation of finishing medical school, tests for medical residency programs and entering the labor market, collaborate to the increase in anxiety and depression symptoms48.
CONCLUSION
It is worth mentioning that some caution must be taken regarding the interpretation of some results of this study, as some questions involved aspects of “intimate nature”, such as sexual orientation and family income. These aspects may have influenced the authenticity of the students’ responses. Even though, as this is a prevalence study, this investigation does not allow conclusions about causality, its results represent an overview of the magnitude of the symptoms of anxiety and depression and their association with demographic, social, economic and behavioral factors. Additional follow-up studies are required to elucidate the course of anxiety and depression in this population group throughout the academic semesters, aiming to present a better understanding of the factors that influence these students’ mental health and to aid in planning interventions to help them deal with the challenges they face.











 texto em
texto em