INTRODUCTION
In the last decades, re-humanizing medicine has received a widespread concern. The influence of the biomedical model, which has been hegemonic for fourteen centuries, promotes a disease-centered approach, instead of a person-centered care1. Since the 20th century, the psychosocial dimension has reintegrated medical education and health practices. It focuses on the construction of a biopsychosocial model, as opposed to the biomedical model. The biopsychosocial model perspective points out the need for doctors to improve their relational skills2. Thus, empathy in the doctor-patient relationship, patient-centered care and humanistic medical care are essential and central professional characteristics and skills for doctors3.
Empathy is a multidimensional construct in the cognitive, emotional and behavioral domains4)-(7. Higher levels of empathy perceived by patients have a positive correlation with their general satisfaction with doctors, interpersonal trust and higher adherence to treatment8, including positive clinical results9. Also, lower levels of empathy are associated to a higher probability of medical error10.
Patient-centered medicine is one of the main methods used to humanize medicine11. It has two principles: person-centered care, which recognizes patients’ ideas and emotions towards the disease; and shared decision-making and responsibilities between doctors and patients related to the disease12. Patient-centered medicine promotes greater patient and doctor satisfaction and reduces (i) adverse effects associated with prescriptions, (ii) complaints about medical care, (iii) volume of complementary exams, (iv) referrals to specialists, and (v) costs to the healthcare system and to the patient11)-(13.
Understanding what precedes empathy regarding the interns’ and young doctors’ attitudes is a relevant topic in the education of health professionals and in their academic and professional performance. Some factors have already been associated to higher levels of empathy and person-centered care, such as the female gender5),(14, the first years of medical school15 and the students’ psychosocial issues in the beginning of the medical course16, working on person-centered medical specialties17 and primary care18. Egalitarianism, global self-esteem and well-being are positively related to empathy and a patient-centered attitude19. Two studies with medical students analyzed spirituality and empathy as correlated variables20),(21. Another study showed a positive association between spirituality, care and empathy22. A recent study associated quality of life to spirituality in medical students and showed that the component meaning and purpose in life was related to higher levels of empathy20. No studies were found associating spirituality or spirituality-related quality of life to patient-centered attitudes in the doctor-patient relationship.
Thus, many associations can be established regarding doctors’ attitudes and behaviors in the doctor-patient relationship. However, the relationship between behavioral and cognitive aspects - such as spirituality, religiosity and personal beliefs - with empathy and attitudes in the doctor-patient relationship needs clarification. Concerning the importance of this issue in medical education, this research assesses how the perception of well-being (quality of life) related to spirituality, religiosity and personal beliefs are associated to medical interns’ and residents’ empathy and attitudes in the doctor-patient relationship. Our hypothesis is that the perception of well-being (quality of life) related to spirituality, religiosity and personal beliefs precedes empathy and the patient-centered care in the doctor-patient relationship.
METHODS AND MATERIALS
Participants
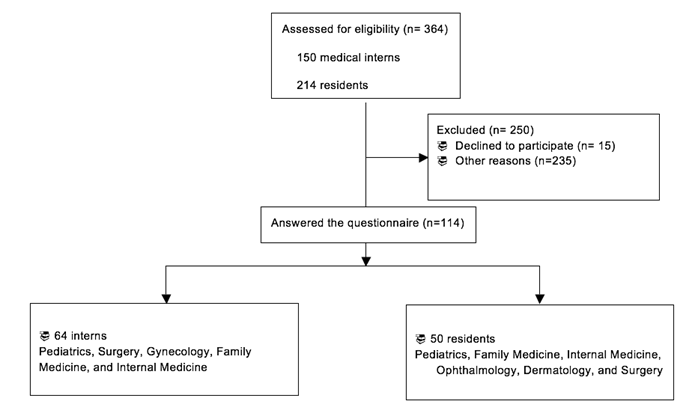
The local research ethics committee of the Federal University of Uberlândia approved this cross-sectional, quantitative study. A total of 150 medical interns attending the fifth and sixth years of medical school and 214 first- to fourth-year residents in the Clinical Hospital of the Federal University of Uberlândia, Brazil, were eligible for the study. Participant selection was carried out by convenience. Participants were 18 years of age or older.
Instruments
The following instruments were used:
The Brazilian version of the World Health Organization Quality of Life - Spirituality, Religiosity and Personal Beliefs (WHOQOL-SRPB) field-test instrument, is a translated, validated, and cross-culturally adapted, self-administered tool23. It consists of 32 questions focused on aspects of quality of life related to spirituality, religiosity and personal beliefs. Individual items are rated on a 5-point Likert scale, providing eight scores/components: Spiritual Connection, Meaning and Purpose in Life, Experiences of Awe and Wonder, Wholeness and Integration, Spiritual Strength, Inner Peace, Hope and Optimism, and Faith. The scores range from 20 to 100. This instrument assesses spiritual, religious or personal beliefs as components of quality of life. Higher scores represent a higher level of positive perceptions of quality of life regarding the SRPB domain24.
Patient-Practitioner Orientation Scale (PPOS)25),(26. It is a self-administered instrument that assesses the attitudes of patients, doctors and medical students regarding the doctor-patient relationship. It has been validated and translated into Portuguese with appropriate psychometric properties27. This scale has 18 items arranged into (i) items related to the dimension of Sharing and (ii) items related to the dimension of Caring. Items are rated in a 6-point Likert scale. Low scores (≤ 4.57) indicate a doctor-centered orientation (high medical control focused on biomedical issues), whereas high scores (≥ 5.00) indicate a patient-centered orientation (shared control and focus on the person as a whole). Scores between 4.57 to 5.00 indicate a partially patient-centered orientation.
The Jefferson Scales of Empathy (JSE)28 measures the empathy of medical students and residents. The instrument has 20 items and three domains: Compassionate Care, Perspective-taking, and Walking in Patient’s Shoes. The possible answers are rated in a 7-point Likert scale. Empathy is as high as the sum (20 to 140) of the answers to all items, with a maximum score of 140 points. The version for medical students (JSE-S Version), validated to be used in Brazil29, was designed to reflect students’ orientation or empathic attitude in medical care.
The Cronbach’s alpha coefficients of the validated questionnaires are: WHOQOL-SRPB (0.879), PPOS (0.714), and JSE (0.805).
A sociodemographic questionnaire identified age, gender, marital status, religious affiliation, current year of medical school, current specialty (residents) or intended specialty (interns), and religious involvement (low or high). All questionnaires were self-administered.
Procedures
Medical interns and residents were approached during outpatient activities in the Clinical Hospital of the Federal University of Uberlândia and in the Primary-Care Health Centers after prior authorization of the responsible professor/preceptor. They were invited to answer the WHOQOL-SRPB, PPOS and JSE scales and a socio-demographic questionnaire, all self-administered.
The intended and ongoing specialties were stratified into person-centered and technology-centered ones18.
At Federal University of Uberlândia, the Medical School program lasts six years, of which the first three are the preclinical years and the last three are the clinical years. The pedagogical model is structured into modules. Knowledge is subdivided into two distinct stages - basic and curricular internship -, and most of the learning scenarios are restricted to the hospital environment.
Statistical Analysis
Descriptive statistics characterized the sample and determined the measures of central tendency and position of the data (mean, median, standard deviation, frequency and percentage). The normality of the data was verified by the Shapiro-Wilks test and the variables will be analyzed considering a normal distribution, as suggested in the literature30. Pearson’s correlation determined the association between the WHOQOL-SRPB (and its subdomains) and all the other study variables (JSE-S and its three domains, PPOS and its two domains, and the socio-demographic data (being an intern, a resident, gender, age, religious involvement). Variables with moderate correlations (r > 0.3)31 with p < 0.05 were used in the stepwise linear regressions. Independent variables: WHOQOL-SRPB (and its domains), gender, age, religious involvement, being an intern, and being a resident. Dependent variables: JSE-S, and PPOS and their domains. R² assessed the goodness-of-fit of the model. Multicollinearity was accepted when the variance inflation factor (VIF) value was >10 and / or when the tolerance score was <0.132. Internal consistency was assessed through Cronbach’s alpha. The software SPSS 20.0 analyzed the data. The alpha level was set at 0.05.
RESULTS
Of the 114 participants, 56.2% are interns attending the fifth and sixth years of medical school and 43.9% are first to fourth-year residents.
The mean age was 25.9 years ± 0.6, with a predominance of female participants (67.5%). Catholicism (44.7%) was the most frequent religion among the participants, as well as high religious involvement (43%) (Table 1).
Table 1 Medical interns’ and residents’ sociodemographic data.
| Variable | N | % |
|---|---|---|
| Sex | ||
| Female | 77 | 67.5% |
| Marital status | ||
| Single | 103 | 90.4% |
| Religion | ||
| Did not answer | 3 | 2.6% |
| Catholic | 51 | 44.7% |
| Afro-Brazilian | 1 | 0.9% |
| Protestant | 13 | 11.4% |
| Spiritism | 21 | 18.4% |
| None | 23 | 20.2% |
| Other | 2 | 1.8% |
| Religious involvement | ||
| High | 67 | 58.77% |
| Low | 47 | 41.22% |
| Medical Interns: Intended Specialty | ||
| Person-centered | 32 | 50% |
| Technology-centered | 15 | 23.43% |
| Did not answer | 17 | 26.56% |
| Medical Residents: Current Specialty | ||
| Person-centered | 45 | 90% |
| Technology-centered | 5 | 10% |
Table 2 shows the mean scores of the JSE-S, PPOS and WHOQOL-SRPB scales. For each WHOQOL-SRPB domain, the lowest and highest mean were Faith (69.29 ± 23.72) and Meaning and Purpose in Life (82.65 ± 13.56), respectively. In the PPOS, the final score (4.59 ± 0.43) indicates a partially patient-centered orientation. The final score of the JSE (118.56 ± 10.25) indicates a number close to the maximum value of 140.
Table 2 Mean and standard deviation of the instruments’ scores
| Variable | Mean | SD | Minimum | Maximum |
|---|---|---|---|---|
| WOQOL-SRPB | ||||
| S1 | 70.40 | 22.92 | 20 | 100 |
| S2 | 82.65 | 13.53 | 40 | 100 |
| S3 | 73.89 | 12.51 | 45 | 100 |
| S4 | 73.60 | 12.91 | 35 | 100 |
| S5 | 72.57 | 18.98 | 20 | 100 |
| S6 | 72.77 | 11.60 | 40 | 100 |
| S7 | 76.16 | 11.58 | 45 | 100 |
| S8 | 69.29 | 23.72 | 20 | 100 |
| Total Score | 74.02 | 12.17 | 36.25 | 99.37 |
| JSE | ||||
| Sub1 | 49.27 | 4.62 | 37 | 56 |
| Sub2 | 8.48 | 2.77 | 2 | 14 |
| Sub3 | 60.81 | 7.13 | 39 | 70 |
| Total Score | 118.56 | 10.25 | 89 | 136 |
| PPOS | ||||
| Share | 4.21 | 0.63 | 2.33 | 5.77 |
| Care | 4.96 | 0.43 | 3.66 | 6.00 |
| Total Score | 4.59 | 0.43 | 3.21 | 5.55 |
WHOQOL-SRPB: WHOQOL- Spirituality, religiosity, and personal beliefs; JSE: Jefferson Scale of Empathy PPOS: Patient-Practitioner Orientation Scale. S1: Spiritual connection; S2: Meaning and purpose in life; S3 Experiences of awe and wonder; S4: Wholeness and integration; S5: Spiritual strength; S6: Inner peace; S7: Hope and optimism; S8: Faith. Sub1: Compassion; Sub2: Walking in Patient’s Shoes; Sub3: Perspective-taking. SD: Standard deviation.
Table 3 shows Pearson’s coefficient correlations between WHOQOL-SRPB (and its domains S1 to S8), JSE-S and its domains, PPOS and its domains, being an intern, being a resident, gender, age, and religious involvement. Significant correlations (p-value < 0.05) varying from weak (r = 0.10) to moderate (r= 0.30) were found. Moderate correlations with r > 0.3 were found: (a) Perspective-taking: Spiritual Connection ( r = 0.309 ; p < 0,01), Wholeness and Integration ( r = 0.342 ; p < 0.01) and WHOQOL-SRPB global score (r = 0.394; p < 0.01); (b) Final JSE score: Wholeness and Integration (r = 0.337; p < 0.01), Inner Peace (r = 0.325; p < 0.01), WHOQOL-SRPB global score (r = 0.352; p < 0.01) ; (c) Sharing : Wholeness and Integration (r = 0.334 ; p < 0.01) ; (d) Caring: WHOQOL-SRPB global score (r = 0.312; p < 0.01) ; (e) PPOS Total score: Meaning and Purpose in Life (r = 0.323 ; p < 0.01), Inner Peace (r = 0.315; p < 0.01) e WHOQOL-SRPB global score (r = 0.358; p < 0.01).
Table 3 Pearson’s correlation coefficients between spirituality, empathy, attitudes and sociodemographic characteristics.
| Variable | Student/ resident | Age | Gender | Religious involvement | S1 Connection | S2 Meaning and purpose in life | S3 Experiences of awe and wonder | S4 Wholeness and Integration | S5 Spiritual strength | S6 Peace- Harmony | S7 Hope | S8 Faith | WHOQOL-SRPB Global score | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| JSE | ||||||||||||||
| Final Score | (r) | -.117 | -.093 | .203* | .222* | .237* | .252** | .272** | .337** | .250** | .325** | .191* | .199* | .352** |
| Sub1 | (r) | -.141 | .102 | .206* | .166 | .072 | .122 | .088 | .175 | .091 | .226* | .113 | .044 | .144 |
| Sub2 | (r) | -.066 | .048 | .023 | -.094 | -.037 | .121 | .071 | .066 | -.021 | .075 | .108 | .066 | .041 |
| Sub3 | (r) | -.051 | .086 | .149 | .248** | .309** | .236* | .306** | .342** | .309** | .291** | .160 | .283** | .394** |
| PPOS | ||||||||||||||
| Final Score | (r) | .123 | .071 | .163 | .115 | .189* | .323** | .336** | .364** | .233* | .315** | .266** | .164 | .358** |
| Share | (r) | .087 | -.029 | .114 | .129 | .122 | .269** | .289** | .334** | .151 | .275** | .212* | .097 | .283** |
| Care | (r) | .121 | .185 | .161 | .043 | .201* | .257** | .255** | .246** | .250** | .236* | .228* | .190* | .312** |
* p<0,05 **p<0.01. WHOQOL-SRPB: WHOQOL Spirituality, religiosity, and personal beliefs; JSE: Jefferson Scale of Empathy PPOS. Patient-Practitioner Orientation Scale. Sub1: Compassion; Sub2: Walking in Patient’s Shoes; Sub3: Perspective-taking.
The results and coefficients after multiple regression analysis (stepwise) are depicted in Table 4. In the final regression model, the following variables were significantly associated: (a) Perspective-taking: WHOQOL-SRPB global score; (b) Compassion: Inner Peace and Gender; (c) Final JSE Score: WHOQOL-SRPB global score; (d) Sharing: Wholeness and Integration; (e) Caring: Meaning and Purpose in Life; (f) Total PPOS Score: Meaning and Purpose in Life. Multicollinearity was not a problem in the regression model when verifying both VIF and tolerance scores.
Table 4 Multiple linear regression analysis of variables moderately correlated with the components and total score of WHOQOL - spirituality/religiosity/personal beliefs and sociodemographic characteristics
| DEPENDENT VARIABLES | INDEPENDENT VARIABLES | Constant | R2 | Adjusted R2 | F | pvalueF | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Perspective-taking | 43.62 | .15 | .14 | 19.64 | .00** | β | pvalueβ | VIF | Tolerance | |
| WHOQOL-SRPB Global score | .39 | .00** | 1.00 | 1.00 | ||||||
| Compassion | 39.47 | .09 | .07 | 5.45 | .01** | β | pvalueβ | VIF | Tolerance | |
| Sex | .20 | .03* | 1.00 | 1.00 | ||||||
| S6- Inner peace | .22 | .01** | 1.00 | 1.00 | ||||||
| JSE Global score | 96.65 | .12 | .11 | 15.16 | .00** | β | pvalueβ | VIF | Tolerance | |
| WHOQOL-SRPB Global score | .35 | .00** | 1.00 | 1.00 | ||||||
| Share | 3.05 | .10 | .09 | 12.72 | .00** | β | pvalueβ | VIF | Tolerance | |
| S4-Wholeness and Integration | .32 | .00** | 1.00 | 1.00 | ||||||
| Care | 4.05 | .11 | .10 | 13.06 | .00** | β | pvalueβ | VIF | Tolerance | |
| S2-Meaning and purpose in life | .33 | .00** | 1.00 | 1.00 | ||||||
| PPOS Global score | 3.53 | .14 | .13 | 18.08 | .00** | β | pvalueβ | VIF | Tolerance | |
| S2-Meaning and purpose in life | .38 | .00** | 1.00 | 1.00 |
* p<0,05 **p<0.01. WHOQOL-SRPB: WHOQOL Spirituality, religiosity and personal beliefs; JSE: Jefferson Scale of Empathy; PPOS: Patient-Practitioner Orientation Scale
DISCUSSION
This research assessed the perception of well-being related to spirituality, religiosity and personal beliefs and its association with empathy and attitudes of medical interns and residents in relation to the doctor-patient relationship. According to our hypothesis, empathy and patient-centered attitude were in general significantly associated with well-being related to spirituality, religiosity, and personal beliefs. The spiritual quality of life predicted the final scores of empathy and perspective-taking. The component meaning and purpose in life predicted the global patient-centered attitude. In addition, inner peace predicted compassion, while wholeness and integration predicted the domain sharing of the patient-centered care.
Spirituality and Empathy
This study found that levels of empathy were positively associated with the perception of well-being related to spirituality, religiosity, and personal beliefs. WHOQOL-SRPB Final Score predicted the global empathy and perspective-taking. Inner peace predicted the domain compassion of JSE. Other studies have found a positive association between spirituality, care, and empathy22),(42.
Previous studies have described that burnout is inversely correlated to empathy, while personal well-being and quality of life showed a positive correlation with empathy scores in medical students7),(43. A recent study with a sample of students has indicated that empathy in the doctor-patient relationship is associated with well-being related to spirituality - Meaning and Purpose in Life20. Therefore, some factors such as well-being7, depression43, and burnout44 are correlated to empathy, supporting the idea that empathy is not only an isolated cognitive dimension.
The perspective-taking of empathy - the cognitive dimension - shows a larger number of associations with the perception of well-being related to spirituality and its components. It means that the cognitive dimension of empathy - the ability to consider the perspective of others10 - is related to factors connected with satisfaction with spirituality/religiosity/inner beliefs of medical interns and young doctors. The search for questions about existence and the meaning and purpose in life could give a transcendental meaning to life and work as a strategy to deal with human suffering, reflecting on higher empathic behavior.
Inner peace, a component of the WHOQOL-SRPB, was correlated to compassion. In fact, this study reinforces that the expression of compassion in the interpersonal relationship stimulates us to understand we are part of a whole, which could be related to the feeling of inner peace45. The inner peace aspect, which integrates the component of spirituality, is defined as: “The source of this peace comes from within the person and may be linked to the relationship that this person has with God or may originate from this person’s belief in a moral code or a set of beliefs”24. Also, gender was a predictive factor in the compassion domain of empathy. Our study replicates the tendency described in the literature on the existence of higher empathy levels in female medical students5),(14. Previous studies have suggested that women are more receptive to emotional cues than men. This quality may contribute to a better understanding of others and a better empathic relationship with the patient25, as well as to the female socialization skills26.
Empathy and religious involvement showed a weak correlation. The multivariate regression analysis indicated that the perception of well-being related to spirituality, religiosity and personal beliefs predicted empathy. This result better explained the model in relation to religious involvement. Previous studies have pointed out that religiosity has an association with better mental health results29),(46, but other studies have shown no association between religious beliefs and empathy31),(22. Religiosity is defined as how much an individual believes in, follows and practices a religion. It may be organizational (to attend a church or a religious temple or non-organizational (to pray, read books, watch religious TV shows)32. Having a religious affiliation or religious involvement was not equally associated with empathy as some domains of spirituality were.
In this sense, when we consider medical education and the empathy approach, we need to broaden the focus and search for other factors that influence students’ and young doctors’ empathic behavior towards patients. The following ideas may provide essential conditions for professional education33 and affect their practice - empathic behavior activities during medical training that stimulate the study of spirituality by acknowledging people’s subjectivity, resources to understand self-care and self-knowledge, and debates about transcendence, inner peace, mechanisms of resilience, and topics on physicians’ well-being. Moreover, such activities may be a mechanism used to face stress, to keep oneself highly resilient and to improve the quality of life34 of interns and residents. Medical schools all over the world have come together to include spirituality in their medical curriculum35)-(37.
Spirituality and Patient-centered Medicine
Our study indicated a positive association between the perception of well-being related to spirituality/religiosity/beliefs and a more patient-centered medical attitude in a sample of medical interns and residents who have been training their skills in clinical practice. Meaning and purpose in life predicted the patient-centered care - PPOS global score - and the Caring domain. Wholeness and integration were a predictor factor of the PPOS Sharing domain.
If empathy is a critical factor for promoting patient-centered care38, and some studies have shown that it is also related to spirituality39),(20, the perception of well-being related to spirituality has an association with patient-centered care, as identified in our study. Research studies have described that doctors’ spirituality and religiosity influence clinical decisions, as well as the doctor-patient relationship40.
This study demonstrates that the component wholeness and integration is associated with sharing. Sharing concerns whether power and control should be shared between the doctor and the patient and to what degree doctors should share information with their patients41. Wholeness and integration regards, for example, “to what extent do you feel any connection between your mind, body and soul? How satisfied are you with having a balance between mind, body and soul? To what extent do you feel the way you live is in accordance with what you feel and think? How much do your beliefs help you create coherence (harmony) between what you do, think and feel?.” Thus, the balance among these three dimensions (body, mind and soul) and the help of beliefs as a mechanism to seek harmony can provide a patient-centered care on sharing decisions and responsibilities between doctors and patients with common goals regarding the disease.
This study highlights the association of meaning and purpose in life with a patient-centered care, as well as the Caring domain. Caring reflects whether participants consider patients’ expectations, feelings and emotions as critical elements41. This study demonstrates that participants report that the component meaning and purpose in life as one of the most important of the WHOQOL-SRPB instrument. Meaning and purpose in life concerns, for example, “to what extent do you find a meaning in life? To what extent does caring for others provide meaning in life for you? To what extent do you feel that your life has a purpose? How much do you feel you are here for a reason?”. In essence, caring for others - caring for the patient - will enable a meaning or purpose in life, and, at the same time, having meaning and purpose in life can provide a more patient-centered care. This is still an unexplored topic in medical schools.
Thus, this study indicates that having a more patient-centered care may not only require training throughout the program stages, but also knowledge and more experience in some domains of spirituality, especially those related to purpose and meaning in life. Therefore, (i) an approach in the context of medical education focused on the medical student’s spirituality, (ii) activities that stimulate finding a meaning and purpose in life and possible devices to help develop them, and (iii) understanding how to deal with emotions and expectations can produce perceptions of positive well-being related to spirituality. They can also result in patient-centered care in the doctor-patient relationship.
Study Limitations
We used self-administered questionnaires on empathy and doctor-patient orientation, which can be influenced by the bias of social desirability, biasing the responses of interns and residents to what is socially accepted. However, this limitation and subjectivity of responses is inherent to this type of study.
Another limitation concerns the sample restriction to the interns attending the last two years of medical school and residents in the first four years of residency, so the data does not represent the other students. New studies have included students attending the first years, as there are indications that this period in higher education is a significant predictor of higher levels of empathy20.
There is also the risk of selection bias - 31.3% of eligible individuals participated in the study. The number is appropriate, but there may be a “Healthy entrant effect” which, in this case, may mean that more empathetic, more religious and spiritualized students are more likely to answer the questionnaire than less empathic and religious ones. In this sense, 67.5% of the study participants were women; 90% of medical residents and 50% of medical interns had chosen or intended to choose a “person-centered” specialty. Therefore, the selection bias can be justified by the fact that the majority of the sample consists of women and students and doctors with a choice of “person-centered” specialties, factors that are related to higher levels of empathy, according to previous studies5),(14),(16.
Although the response rate was satisfactory for the eligible individuals (31.3%) in this study, the research was carried out in a single higher education institution and thus, external validity was not verified. However, the total WHOQOL-SRPB score (74.02) in our study group is similar to the results of other studies20 (ranging from 71.76 to 73.5) in a similar population - medical students in Brazil - which reinforces the appropriateness of the selection method and the sample size.
CONCLUSION
Well-being related to the spirituality of the medical interns and residents has a positive association with patient-centered care and empathic behavior. This study enhances our understanding on the need to consider spirituality and beliefs in medical education. Debates on these issues, especially on the meaning and purpose in life and inner peace as part of the medical curriculum, might lead to better results in the humanization of medical practice.