INTRODUCTION
Medical teams constantly work with patients in critical conditions and complex environments. Within these environments it is understood that cognitive, metacognitive, and affective processes coexist, providing or preventing an adequate performance1),(2. During medical emergencies, adverse events and life-threatening errors commonly occur. Studies have shown that there are several cognitive errors9 in clinical decision-making that may occur due to diagnostic uncertainty, the novelty of the case and the frequency of specific distractions from medical emergencies, and they may also occur as a result of communication difficulties10),(11.
Realistic simulation is an active teaching-learning methodology that facilitates training by approximating , real scenario12. Despite the potential benefits of training using simulation, more research is needed to assess the nature of learning and performance in simulated environments13)-(15.
In this context, it is believed that the realistic simulation, through simulated scenarios, can develop the metacognitive skills and experiences of doctors, resulting in gains when dealing with the complexity of the diagnostic task, given the uncertainties of the cases, hypotheses and alternatives in decision-making.
Therefore, we seek to address the following research questions:
What is the nature of the metacognitive processes of a team of medical students who face difficulties with a medical emergency simulation?
What contributions can metacognitive processes bring to the medical teaching?
Metacognition can contribute since it is understood as knowledge about the cognitive processes and products themselves. Due to the scarcity of research in this area, the present study sought to achieve two objectives. First, it aimed to explain the failure of a knowledgeable team of medical students in attending a medical emergency simulation, describing and interpreting the nature of their metacognitive processes. Second, , it sought to establish possible contributions of these processes to the medical teaching.
METHODS
Scenario
The simulation took place in a “simulation contest for attending critical patients” at a national medical education congress. This contest has been a regular pre-congress event of the Brazilian Medical Education Association (ABEM, Associação Brasileira de Educação Médica). It uses clinical simulation scenarios, based on the construction of the National Examination for the Revalidation of Medical Diplomas Issued by a Foreign Higher Education Institution (Revalida) test stations. These scenarios are created by medical school professors from the city where the congress is held, guided by another professor from the national association simulation program. Enrollment required medical students, on a voluntary basis, to organize themselves in attending teams to participate in the contest.
The simulation used a high-fidelity mannequin and the physical environment. The equipment was appropriately structured for an emergency, The mannequin is offered by a company that participates in the congress in partnership with ABEM.
To evaluate the performance of the enrolled teams, a judging commission, consisting of three professors, watched the performed simulated care. Therefore, it was possible to observe the events and control the duration of the scenario (the same for all scenarios and teams), as well as, eventually, determine its early ending. There was also a facilitator, who remained inside the simulated environment and who was responsible for meeting the demands of the team, such as requests for complementary exams, information not provided by the scenario, among others.
Two different teams competed in the same simulated station, with the first team being confined (without communication), without watching the other team’s performance. The participating teams were asked to make all communications out loud, as well as the diagnostic hypotheses, reasoning and reasons that justified the different conducts and procedures, as well as any requests made. The main criterion for judgment was the correctness of the diagnostic hypothesis and its corresponding treatment. After each scenario was over, the team, based on its performance, could be eliminated from the competition or proceed to the subsequent scenarios, created with an increasing degree of complexity at each stage.
The simulated stations were public and took place in two rooms, where, in addition to the already mentioned components, there were places for audiences consisting of other participating teams and spectators, usually congress attendees in some way connected to the topic or to the members of the teams.
Description of the case study
For this study, we intentionally selected the contest’s winning team. Because they failed to carry out the medical diagnosis and, consequently, the treatment, the team was eliminated when it participated in the first simulated scenario. However, they returned to the competition due to the opportunity they had in the recap, and in the end, it was declared the winner of the contest. So, it is interesting to explain how a team capable enough to win, fails at first.
In this study, only the the team’s first performance, where the misdiagnosis occurs, will be analyzed. The clinical case presented to the team consisted of a woman with pulmonary thromboembolism. However, the team attained a diagnosis of acute coronary syndrome and made all relevant interventions for its treatment.
The study participants were components of the winning team of the contest, consisting of four medical students from a private medical school, enrolled in the eighth semester, aged between 23 and 26 years. For the purposes of this study, the team’s capacity was considered adequate due to its level of training and the fact that, under equal conditions, it surpassed all other competitors.
Type of study
This is a case study, with a qualitative design, aiming to describe the events that led to the misdiagnosis made by medical students during their participation in simulated critical care scenarios. The study was registered with the Research Ethics Committee of Institute of Collective Health Studies at the Federal University of Rio de Janeiro under number CAAE 96007018.5.0000.5286 and approved by Opinion n. 2,938,945, dated of October 4, 2018.
In the approved project, among other purposes, we registered our intention to use the congress as a study environment, as well as the detailed description of the ethical and methodological aspects. ABEM and the National Medical Education Congress Commissions had prior knowledge of the study and approved it. To preserve the subjects’ anonymity, the original names were replaced by pseudonyms.
Data collection
The simulation contest was held as a pre-congress event and the interview was held on the last day, after the contest results were made public. The collection technique was the group interview3, which was recorded and transcribed. It was performed in a group, in a comfortable and private environment, and the questions were directed most of the time to the group as a whole. In some cases, looking for specific clarifications, a question was addressed to a particular subject.
The interviewer did not use a list of previously prepared questions. They preferred to be guided by an intentionally vague script (Table 1). Then, according to the direction indicated by the participants, the interviewer, guided by the focus of the study, progressively asked other questions that sought, at times, to detail events, and sometimes, to clearly express thoughts. Thus, they directed their questions seeking to unveil, from a metacognitive point of view, the thought processes that modulated the team’s performance, leading to a misdiagnosis and its consequent early elimination. More specifically, they tried to understand why the team was eliminated in the first scenario, given that, due to the recap, it was able to continue in the competition, proving itself capable enough to win.
Table 1 Interview script.
| Steps to be detailed during the interview |
|---|
| Personal and research team presentation. |
| Presentation of the study and formalization of ethical aspects. |
| Request for consent by through the FICF. |
| Presentation and identification of the subjects and their consent to the FICF |
| Expectations regarding the contest. |
| Team characteristics and formation. |
| General team behavior during the contest. |
| Details of the circumstances and events associated with the misdiagnosis. |
| Participants’ evaluation regarding their participation in the contest. |
Source: Elaborated by the authors.
Data analysis
The metacognitive theory5),(16 was used for content analysis4. Metacognition is:
“a broad term, used to describe different aspects of knowledge that we build about how we perceive, remember, think and act. A capacity to know about what we know. It is, therefore, a second-level discourse about knowledge, characterized as a system of thought focused on human cognitive activity (p. 69-70)16.”
We applied the content analysis technique to the interview4 in four sequential stages. In the first stage, the interview was recorded and transcribed to a text file. In the second stage, which is the skimming reading, the text was repeatedly read by the interviewer to understand the global meaning of the events, as well as the specific roles of the subjects and their relationships in the group.
In the third stage, the text was coded using the qualitative analysis software Atlas-ti™, according to the metacognitive variables of Efklides5, understood in this study as theoretical categories. In this stage, the global meanings perceived before were translated into terms of metacognitive variables. Thus, at the end of this stage, there was a list of all the parts that showed metacognitive activity, encoded by the corresponding metacognitive variable.
In the fourth stage, we tried to answer the guiding question of the research. Using the SimpleMind© Mind Map Editor, the produced material was arranged in two steps.
In the first step, the parts of the speeches expressing metacognitive activity were arranged in chronological order. In this way, it was possible to show a process that, starting from an initial diagnosis, proceeded with an unfavorable evolution of the case until the critical incident that, in the end, signaled failure for the team.
In the second step, we linked each moment of this chronology to the corresponding metacognitive variable, which had been identified in the third stage. In doing so, we were able to describe, from a metacognitive perspective, the thinking process that explained why a capable team failed where it was not expected.
The primary analyzed outcome was the presence of metacognitive events in the research subjects’ speeches. The secondary outcome was the demonstration/description of a significant role of the metacognitive processes in the performance of the teams participating in the contest.
RESULTS AND DISCUSSION
The following results will be described as text. As previously mentioned, in the first scenario, the team, faced a Pulmonary Venous Thromboembolism (PVTE) clinical condition, misdiagnosed the case as Acute Myocardial Infarction (AMI). To understand the process that led to the error, it is necessary to look at a time before the contest.
It starts when the group organizes itself to participate and does it in a serious and capable way. The process of choosing participants and team composition is the subject of another future study.
What matters here is that having formed as a team, the group evaluated the conditions and rules of the contest and, preliminarily, predicted a set of possible scenarios. Among them was AMI. Which makes sense, given that the competition would be about care of critically-ill patients.
This is the moment when one can identify the use of the Metacognitive Ability(a) (MA) of Prediction(b). Thus:
[Mariana] Since the beginning we were thinking like that ...
[Francisco] What would come to us ...
[Mariana] We already had Coronary Syndrome in mind.
Having made the prediction, and in a manner consistent with it, the group plans and anticipates what they will do. At the same time, watching the participation of other teams, the new information supports and ratifies the developed reasoning.
In this sense, the use of Planning MA(c), in a way, led to the attainment of a diagnosis that was defined even before they knew anything about the real case.
[Francisco] Mariana and I entered with Coronary Syndrome in our heads, and we wanted to fit this into the patient...
[Francisco] I think this was what got in the way, because we were the third case, ... and we knew that if a Coronary Syndrome came to us, we knew how to manage it well, so we were prepared...
[Carlos] That was the subject we discussed during the interval between scenarios and then we took it and reviewed what each one knew...
It is important to note that initially, in the scenario of PVTE, the diagnosis of AMI was also possible. The first data allowed this diagnostic hypothesis.
The initial scenario could then be interpreted as originally predicted. It is, therefore, the moment when the Metacognitive Experience(d) (ME) of Familiarity(e) elicits the ME of Feeling of Confidence(f) (FC). Therefore, the team feels comfortable in continuing with the care, even with an inadequate diagnosis in their hands.
[Francisco] Then a case came for us of a patient with chest pain...
[Mariana] I think that Coronary Syndrome, at least that was what I saw the most in real patients ... and you think, chest pain, cough sometimes, but it is not associated, so you end up memorizing it more because it is more common, more frequent in care.
[Francisco] Then there were the four of us and we started investigating that and I wanted to fit in here anyway, because the differential diagnosis does not change...
Up to this point, although biased, the thinking process occurs without the team noticing any greater difficulties. Based on the assumption of an AMI scenario, the team, even if omitting aspects that are relevant to the correct diagnosis, confirms the original diagnosis by privileging the biased selected signs and symptoms. This results in a generalized Feeling of Confidence in the team, which feeds back both the original diagnosis and the subsequent therapeutic procedures.
As Terra-Filho et al17 state: “Due to its multifaceted clinical picture and its often silent nature, PVTE is a disease that is still enigmatic from an epidemiological point of view.”, constituting an important health problem in Brazil. Between 1989 and 2010 there were approximately 92,000 fatal cases, of which 55.8% were women, with the mortality rate standardized by age in 2010 of 2.62/100,00018. It should be noted here that the diagnosis of PVTE is neither simple nor immediate. In acute cases, the differential diagnosis includes cardiac tamponade, acute myocardial infarction, aortic dissection, acute valve dysfunction and hypovolemia19. It is estimated that, in the United States, it is the third leading cause of death in hospitalized patients and, despite this, the majority of cases are not diagnosed while the patient is alive. Moreover, less than 10% of fatal cases received specific treatment for the disease20. In Brazil, other factors that hinder the diagnosis are the overlapping of signs and symptoms and also the non-specificity of a good part of the clinical condition21)-(24. Figure 1 shows a summary of this context.
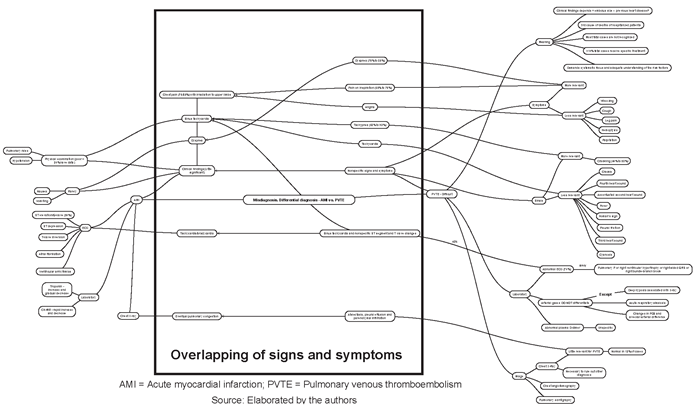
Figure 1 Summary of the difficulties of the differential diagnosis between pulmonary venous thromboembolism and acute myocardial infarction.
At that time, as already mentioned, AMI was a possibility, but not the only one. But the first findings were recognized as being indicative of AMI only. This is because the FC inhibited the MA of Error Detection(g) (ED) allowing the continuation of the wrong conduct.
[Jaqueline] That is it and we had one of the cases, which was the most common cases of the practical experience, right? It will be Coronary Syndrome and we had our minds so set on it ... and then the diagnosis was, then there was one more thing, then when the ECG stopped, and we analyzed it wrongly ...
[Francisco] There was a sinus bradycardia but ...
Thus, as the team was unable to monitor the environment, it provided biased information to the meta-level(h), making it difficult to detect the error and, therefore, inhibiting the MA of Evaluation(i), which could correct it. In other words, there had no environment monitoring and control to verify clinical prediction.
[Mariana] It does not fit into what we were thinking, but, what else can we think that we are failing to see? ...
[Jaqueline] And even inside the case, we ended up omitting the x-ray that would change the diagnosis.
[Mariana] The only difficulty was the lack of response that we were focused on. And the mistake was not to stop and think.
[Jaqueline] It is just that we saw part of the diagnosis, we focused on a diagnosis and you forget the total complaints like those of the patient.
[Carlos] At that moment we believed that it was a Coronary Syndrome and it was ongoing, the coughing and the fact that the patient was a smoker was a coincidence ...
[Francisco] And none of the four thought about the PVTE ...
[Jaqueline] It was like that, we did not stop and reanalyzed the case, we went on like this and going on with our mistakes, went on erring and went on with our mistake. We did not stop and reevaluate the situation and ... we stopped like that at the end and said, “dude, no, let’s think about what is going on” then it was too late and the scene was over.
In Medicine, it is not possible to proceed with an error with impunity. The negative evolution of the clinical condition shows the weakness of the previous FC. The patient’s inadequate responses (from the perspective of what the team expected) reduce the previous Feeling of Confidence, when the ME of the Feeling of Difficulty(j) arises.
[Jaqueline] Until the moment the patient did not progress well, then ...
[Carlos] The patient developed bradycardia and ... and that ended the scenario.
[Jaqueline] But we were not like ... “because she was not showing a good response, like she was supposed to do” instead of analyzing what was happening we were “wow, but she is not responding” ...
[Francisco] We did not express this clearly, but only at the end of the scene, we were sure it was not Coronary Syndrome and it was an unknown situation, like ... at the opposite times, we did not know what to think.
The situation was one of difficulty and lack of response from the patient to the prescribed therapy. For the team, that was clear. But, despite this, they persisted, looking only for data that would confirm the original diagnosis of AMI and distorting the MA of Monitoring(k) and Control(l), thus resulting in the impossibility of using ED and Conflict Resolution(m) (CR) strategies by activating the Working Memory(n) (WM). In other words, the team did not stop what they were doing to try to realize and resolve what was wrong. And, here, an initial solution would have been to seek in their memory that other differential diagnoses could explain the current situation.
Therefore, the team does not transform the Feeling of Difficulty into a correction tool. That is because of two reasons. On the one hand, in practical terms, due to the closing of the case by decision of the judging panel. On the other hand, this “freezing up” in the difficulty is explained by the fact that the inadequate control continues to pose a bias to the observation, preventing the detection of the error and the resolution of the conflict between the team’s expectation and the patient’s evolution. This conflict could have been resolved, as already mentioned, by activating the WM.
[Carlos] There was a moment when we even mentioned that when we made the decision to intubate the patient, she insisted that “ah, isn’t it because I’m a smoker, doesn’t that interfere?” and she insisted in the fact that she was a smoker three times, then I stopped and I thought “no, but smoking and chest pain due to Coronary Syndrome, she will respond and she won’t...” so, it was at that moment that I stopped, I separated this issue of the coughing and the smoking, but this was what stood out to me, the insistence, it seemed there was something that pulled me in that direction, so that I could pay attention to the smoking ...
[Carlos] I realized that I had to pay attention to the smoking, ... but I could not find it anywhere and I ignored it.
[Mariana] It seemed like it was left over…
[Jaqueline] But there was something bothering us, we knew that a piece was missing, ... like this ...
[Mariana] It’s like, the puzzle is complete but, and this smoking, and this cough ...
[Interviewer] But was there a feeling of something bothering you, somehow?
[Jaqueline] Yes, there was, not only after it was over, it was there. Because the exams were normal, it did not fit in, but at the time, I think it was the ...
[Francisco] There was also nervousness about the first case ...
[Jaqueline] Yeah, that was it, in the first case, it was nervousness that had the most impact on us, we couldn’t think, at the time, there was a great deal of nervousness, I wasn’t prepared like that ...
By decision of the judging panel, the scenario was finished. If there had been more time, could this narrative have had a better outcome? It is difficult to know, but there are positive indications. Throughout the process, there were several signs and symptoms that could have led to the correct diagnosis, but for the reasons already explained, they were eliminated from the main line of reasoning. However, they added up and generated a state of uncertainty and anxiety. And finally, there was a picture of bradycardia, which acted as a critical incident for possible course correction.
As mentioned, the team started the process with a preconceived diagnosis and thus remained for most of the time, with the already described distortions and biases in the metacognitive variables. And the error perception was not attained instantly. Throughout the simulation, the team was vaguely and imprecisely constructing this perception. During this period, several conditions and data were accumulated {*}, being expressed as the Feeling of Difficulty. The culmination of this process was the occurrence of bradycardia (critical incident), which was configured as the effective and instantaneous condition {**} to pay attention to the existence of the error. At this moment, the examining board decided to finish the scenario {***} preventing any actions and thoughts arising from the critical incident.
{*} [Francisco] I think that from the moment the anamnesis data ... There were no ECG findings that we would like to see, laboratory data that we would like to see, maybe a typical pain that we would like to see, since the beginning, clues that told us and that it was not... {**} It is that it was decisive (the bradycardia) but, {*} from the moment the anamnesis data, the tests that we requested that did not match what we were thinking ... {*} But it was this difficulty that made us keep investigating things that ...
[Mariana] {*} And we requested all the extra exams
[Interviewer] There were some signs that you noticed and added up ...
[All] {**} Up to the point of the bradycardia.
[Mariana] {** }For me, at least, {*} some anxiety, like, “I am doing what I know. What is it that it is not working? What am I doing wrong? ”
[Carlos] {**} The decisive moment was the bradycardia that could not be resolved and from that moment on we said, “no, it is wrong”
[Mariana] {**} The bradycardia started…
[Francisco] {**} That is what led us to the perception…
[Carlos] {***} The patient developed bradycardia and (inaudible 19m46s) and then the scenario was over.
To conclude this narrative, let us imagine another outcome, where hypothetically the error would be corrected through the following sequence of actions and reasoning:
The bradycardia demands MA for Selective Attention(o) for differential diagnoses.
For this purpose, Control is activated to monitor the scenario, inhibiting the current actions by Inhibitory Control(p) and reorganizing the framework so that the Working Memory could provide differential diagnoses for Conflict Resolution between:
Up to this point, in the metacognitive perspective, what has been described here is the thinking process underlying the actions. It is now necessary to contextualize this study in the broader perspective of medical education. We have already pointed out the realistic simulation as an active methodology12. It should also be placed in the domain of problem-solving methodologies, differentiating it from the problem-based learning6. In this study, we are closer to the first case, since, in the simulation, the context seeks to mirror reality, both in terms of the physical and social environment, as well as in the specific content to be worked on. Moreover, and mainly because the problem arises from the real scenario. According to Maia25:
When reality problematizing, a cut-out of the world (real or, at least, credible) triggers the student’s learning, by bringing them closer to the study of a real clinical situation, and not of a topic or content whose applicability in their practice is not clearly situated. It is not simply an addition of knowledges to those previously built, but the establishment of new and eventually complex networks between learned concepts.
Highly recommended in these cases is the Maguerez Arch, guiding a pedagogical cycle that takes reality as its starting and ending point, where between one and the other the student observes, selects the relevant aspects, resorts to theory and creates hypotheses for the solution, which are finally tested in reality. Therefore, it is possible to return to theorizing, only now more dense and grounded in reality6.
We suppose there is a strong overlap between the Arch and the simulation processes when the term “reality” is replaced by “scenario”. Therefore, within a simulation, students need to observe the scenario, identify the problem and differentiate the irrelevant from the incidental. Alone, or with the support of the teacher, they interact with the theory for the construction of diagnostic hypotheses and test them, using complementary exams or, at a later stage, applying the relevant therapies.
At the end of the process, during the debriefing, they once again access the theory, now in a more complex and complete condition, as their previous knowledge is integrated with those provided by the teacher and the one that came from the simulated scenario, making them more aware through the debriefing process itself.
In this understanding, the domain of the Maguerez Arch is the cognitive one. Teacher and student sometimes focus on the external environment (the patient, the health system, etc.), and sometimes on the cognitive content, in the form of medical facts and concepts in the theorizing stage. Moreover, its use occurs through a process of interaction between teacher and student, which aims to promote meaningful learning6. In David P. Ausubel’s Subsumption Theory, the meaning of a concept is constituted not only by its definition, but also and mainly by its relationship with all others that are related to it. Therefore, it is of little importance that a student only knows how to define what hypovolemia is. It is more significant that the student be able to do so in the context of the pathophysiology of shock, for instance. And it is only when the learning of a new concept is not carried out by simply adding it to the cognitive structure, but by its reorganization, that meaningful learning occurs7),(8.
That is why the Maguerez Arch is so well-matched with the Ausubelian Theory. In the several stages of observation, construction of hypothesis, theorizing and testing, it constitutes an important instrument for the operationalization of the aforementioned theory in the medical teaching.
When dealing with a metacognitive domain, we address the ability to manage thinking. And, even more, how metacognition can contribute to medical education and, specifically here, to the development of professional competence. And for the purposes of this study, the term is understood as the “circumstantial capacity to jointly mobilize cognitive, psychomotor and affective resources, in order to address or resolve a complex situation (p.205)”6.
Metacognition is more than a simple description of the cognitive process. It has the capacity to manage this process as postulated by the Nelson et al26 model. For the authors, thinking occurs at two levels: cognitive and metacognitive. Ideal functioning models are in the latter, and it is also the latter that monitors the cognitive level. Through monitoring mechanisms, the cognitive level informs the meta-level about the evolution of the processes, and that evaluates its suitability and controls the cognitive level, indicating the maintenance or alterations of the ongoing processes.
It is observed that what joins these three domains is the active and reflective thinking. Therefore, in practical environments, Maguerez Arch it is a relevant resource. To significantly learn is to correlate concepts, and to be competent is to make deliberate choices. Govaerts27, as a matter of fact, is explicit in stating that “knowing is not enough for doing, nor is doing enough for learning: competence require experience and reflection in professional practice at any level of experience(p.235)”.
CONCLUSION
The present study contributes to the medical education literature providing a case study about the metacognitive processes present in a team of medical students attending a medical emergency simulation in the context of a “simulation contest of attending to critical patients”.
It was possible to demonstrate that the simple mastery of the specific content was not sufficient to resolve the proposed complex situation. The adequate medical diagnosis implies sufficient medical knowledge and correct use of clinical reasoning processes. Here, apparently, the error was due not to the lack of previous knowledge, but to reasoning bias. That is, the team focused on a confirmation perspective, without paying attention to discordant signs and symptoms.
The first novelty of this study was to demonstrate, through metacognitive investigation, the possibility of making the process visible. And even more so, at least in this case, being able to explain how and why a specific type of medical reasoning error occurs.
The second, resulting from the first, was to point to metacognition, due to its ability to manage thinking, as an important didactic tool, also allowing the integration of the Maguerez Arch and Meaningful Learning in the search for medical education for competence. Therefore, the collected data go forward into the theoretical field, proposing an integration between four aspects: Metacognition, the Maguerez Arch, Meaningful Learning and the development of competences.
Although the authors are aware that, at this moment, the proposed integration, even if with rationales, is still a conjectural one, they consider its originality to justify its mention in this study. They also understand that the proposal should be further expanded, but this scope is outside the focus and limits of this article and it is intended to be better assessed in future studies.
For this reason, the results of this research provide subsidies both to improve the design and delivery of team-based simulation training, and to improve the teaching and learning processes for medical students and professionals.











 texto em
texto em 



