INTRODUCTION
A high rate of mental disorders among medical students has been associated to a series of factors inherent both to the university context and the individuals themselves, who, upon entering undergraduate school, must deal with issues associated with adolescence, transition to the university, adapting to different learning methods and establishing new interpersonal relationships1)-(3).
In a systematic review study with a meta-analysis in 2017, the prevalence of several mental health problems in medical students in Brazil was verified, including depression, burnout, alcohol abuse and anxiety. Among these, the most prevalent, as well as in the general population, was anxiety, indicating that most medical students in the country have a tendency towards showing anxiety symptoms. The analysis also showed that the students’ signs of depression, when stratified by severity, are predominantly mild2.
A cross-sectional qualitative study, carried out by Tenório et al. in 2016, sought to assess the mental health of 78 students from two medical schools with different teaching and learning models, one of them with a traditional approach and the other structured as Problem-Based Learning (PBL). Using a semi-structured questionnaire and focal groups consisting of students, it was found that the educational process was associated with psychological distress in both groups, who reported motivations, course-related sources of stress, and similar relief factors4.
In this context, in which medical training is often associated with psychological and emotional disorders, the institutions that train medical professionals have an ethical commitment to be concerned with their students’ mental health, offering prevention and care strategies in this area.
In Brazil, the concern of higher education institutions with their students’ mental health status acquired greater relevance in the second half of the 20th century, with the implementation of services that offered psychological assistance to university students. The first service created for this purpose was established in 1957 at Universidade Federal de Pernambuco and had medical students as the first recipients. In the same context, in the 1960s, federal universities in the states of Rio Grande do Sul, Minas Gerais and Rio de Janeiro also implemented mental health services for their students. Since then, several assistance projects aimed at promoting students’ mental health have been implemented in higher education centers in Brazil5),(6.
Aiming to guarantee the success of psychological and psychiatric assistance within the academic environment, the anonymity, independence and the principle of flexibility are considered the main characteristics that assistance services for university students must have. The confidentiality of the information shared during care, the independence of the service in relation to the teaching departments, with an assistance team not connected with the institution, and the flexibility of the type of care offered according to each individual’s circumstances and identity contribute for these services to accomplish the care function with excellence and ethics7.
In 2016, at the 1st São Paulo Forum of Support Services for Medical Students, the “Carta de Marília” was created. In this document, created collectively by representatives of student support services, teachers and students, the responsibility of educational institutions in promoting and recovering the mental health of university students was highlighted. Among the actions that can contribute to this end, actions were elected, ranging from individualized care by qualified professionals to the promotion of cultural activities that go beyond the academic environment8.
However, challenges remain regarding the implementation and expansion of medical student assistance services, which already existed when these approaches were introduced. It has been verified that the current demands of medical schools in the country are associated to the adequacy of care to the individual assistance model and the application of new support strategies, such as the incentive to develop extracurricular activities9.
To contribute to the discussion regarding support services for medical students in Brazilian institutions, it is important to map and learn about existing publications on this type of service, as well as to understand how they work. Thus, we expect to offer subsidies for the improvement of the mental health promotion actions offered by the medical teaching center services and, ultimately, to collaborate for the quality of the care provided to the medical student.
In this sense, this study aims to identify scientific publications on the assistance services offered to medical students in higher education institutions in Brazil, as well as information on the professionals who comprise them, the intended target audience and the types of interventions most frequently used in these services.
Review questions
The following questions guided the research:
What has been published about the mental health support services made available to students in higher education institutions that offer a medical course in Brazil?
What are the strategies adopted by support services to promote mental health?
Which professionals are responsible for providing these mental health support services to the student?
METHOD
Type of study
This is a systematic literature review guided by the “Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA)” guidelines and carried out to identify studies that describe mental health support services provided to medical students, in the context of the Higher Education Institutions in Brazil.
Inclusion and exclusion criteria
All identified studies written in Portuguese, English or Spanish that addressed the existece of mental health support services for medical students in higher education institutions in Brazil, without time limits, but that were published by August 2020, which was the moment of the last search, were included in the review.
Studies dealing with interventions aimed at promoting medical students’ mental health that had not been promoted by a service structured for this purpose were excluded, as well as studies of which access to the full text was not possible.
Databases
A systematic search was conducted based on articles and dissertations published in the following databases: Pubmed / Medline, Lilacs, The Cochrane Library, Scielo, ERIC and CAPES theses and dissertations catalog.
Search Strategy
The search strategy was defined based on an advanced search conducted on these bases, in order to include the largest number of relevant studies. The descriptors used as reference were “Serviços de apoio”, “Saúde mental” and “Estudantes de medicina”, as well as their English correspondents “Support services”, “Mental health” and “Medical students”. The search strategies were adapted for the different databases and are described in Chart 1.
Chart 1 Search strategies
| Databases | Search strategies | Total number of studies found |
|---|---|---|
| PubMed/ Medline | ((((Support services) OR (psychological support)) AND (mental health)) AND (medical students)) AND (brazil) | 20 studies |
| LILACS | (tw:(Serviços de apoio )) OR (tw:(apoio psicológico)) OR (tw:(apoio )) AND (tw:(mental health )) AND (tw:(medical students )) | 31 studies |
| The Cochrane Library | #1 (Support service) OR (psychological support) #2 (mental health) #3 (medical students) #4 (brazil) #5 (#1 AND #2 AND #3 AND #4 AND #5) | 63 studies |
| ERIC | “Support service” “psychological support” “mental health” “medical students” “brazil” | 6 articles |
| Scielo | (ab:(*serviços de apoio)) OR (apoio) OR (apoio psicológico) AND (saúde mental) AND (estudantes de medicina) | 4 articles |
| CAPES theses and dissertations catalog | Serviços de apoio OR apoio OR apoio psicológico AND saúde mental AND estudantes de medicina | 47 articles |
Study selection and data extraction
All references found through the searches were organized using Mendeley Software10. Then, the Cochrane Collaboration’s Covidence Platform for Systematic Review11 was used as a tool for the selection, screening and extraction of study data.
Study selection was independently carried out by two appropriately trained reviewers. The Covidence Platform provides an interface for each reviewer and then indicates which studies showed divergences in the analysis, so they can be resolved by a third reviewer. Initially, the title and summary of the selected texts were analyzed. Disagreements about the inclusion or exclusion of a particular study were analyzed by a third reviewer. After this stage, the evaluation of the complete texts and definition of the species that would constitute the review was carried out. Once again, in case of studies that showed divergences between the two main reviewers, the third reviewer resolved the conflicts.
Data were extracted from the included studies using data extraction tables, designed to meet the objectives of this review. The characteristics of the studies were taken from the abstracts and the full texts of the studies. Two reviewers independently extracted the data and, in cases of divergence, the data were analyzed by a third reviewer.
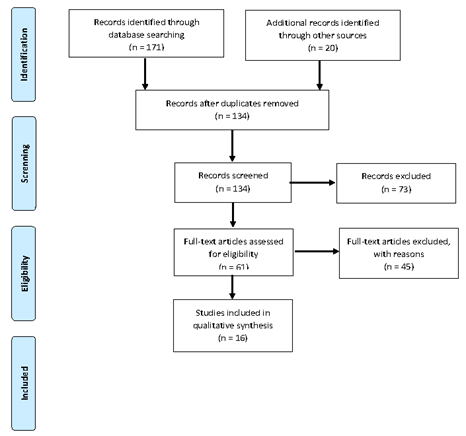
A total of 171 studies were found by searching the databases. In addition to these, another 20 articles were screened, identified in the references of selected studies.
Of the total of 191 selected studies, 57 were excluded by the Covidence platform itself because they were duplicates, leaving 134 studies to be screened based on their title and abstract. The full texts of 61 studies were assessed for eligibility, and after the exclusion of 45 for not meeting the inclusion criteria, the 16 included studies remained (Figure 1).
RESULTS AND DISCUSSION
Characteristics of included studies
Based on the literature search, 16 studies were selected for the construction of this review. Of these, 13 are articles published in journals and three are dissertations presented at postgraduate programs of higher education institutions12)-(14). Regarding the methodological design of these studies, the predominant type was the documentary research of medical records and registration forms made available at the mental health support services. Other identified designs are experience reports15),(16 and historical description17),(18, in addition to qualitative research with the application of questionnaires19 and the phenomenological analysis of testimonials13),(20.
All selected studies were carried out in Brazil, 14 of them involving higher education institutions in the Southeast region. Only two studies were carried out in other locations, one in an institution in the North region16 and the other in a higher education institution in the South region21. Thus, a concentration of publications on mental health support services for medical students in teaching centers in the Southeast region was verified. Moreover, it is noteworthy the scarcity of studies on this topic, especially when compared to the number of institutions offering undergraduate medical courses in Brazil - 287 public and private higher education institutions22.
The data show that 13 of the carried out studies took place in public institutions of higher education and that only three21),(23),(24 were carried out in private ones, which may possibly be the result of a policy of greater incentive to research in public institutions. Studies indicate that the public sector is more structured for performing research than the private sector, due to the educational policies historically adopted in the country. Although there has been greater incentive to private institutions in the last decade, this stimulus was not intended for research, but for professional training25.
Some mental health support services are described in more than one study, such as the Group of Psychological Assistance to Students of Faculdade de Medicina da Universidade de São Paulo (Grapal/FMUSP), addressed in two selected studies18),(26; the Psychological and Psychiatric Assistance to Students of Universidade Estadual de Campinas (Sappe/Unicamp), assessed in the studies by Campos12 and Oliveira14; and the Educational and Psychological Support Center of Faculdade de Medicina de Ribeirão Preto (Caep/FMRP), also described in two studies15),(17. This information corroborates the finding that studies on support services for medical students are concentrated in public teaching institutions in the Southeast region.
Finally, it is worth noting that the studies included in this review analyzed mainly the process of implementing the mental health support service, the characteristics of the offered service, the sociodemographic and clinical traits of the assisted audience, and the main reasons for seeking care in these services.
Creation of services
Each educational institution, when it creates a mental health support service for its students, seeks to meet the demands of their academic context. The Psychosocial Care Space (Epsico) of Universidade do Estado do Amazonas (UEA)16 and the Psychological Assistance Project of Pontifícia Universidade Católica de Minas Gerais (APP/PUC Minas)23 are examples of cases in which the idea of offering strategies to promote mental health came from the management of the academic unit, after verifying situations of psychological distress among the students.
In both cases, the process was similar: faced with an increasing number of students with academic and psychosocial demands related to entering university and adapting to that scenario, a committee of teachers and managers was created to mobilize resources and strategies for the implementation of a student-oriented service.
In addition, it is worth noting that the performance of professors linked to the disciplines of psychiatry and medical psychology were important for the creation of support services in many institutions. The Caep of FMRP17 and the Grapal of FMUSP18, were designed and sponsored by professors who were close to the medical students and understood the need to offer psychological assistance to this audience.
Considering these examples, the importance of the articulation between the academic community and the managers of the medical education institutions is observed in the implementation of support services to their students’ mental health.
Types of offered services and interventions
The mental health support services described in the selected studies are mostly structured to offer a first embracement, such as individual psychological care for a short period of time, in cases of psychological distress related to personal and / or academic issues.
Most services have pre-established hours of operation, and the demand for care is due to spontaneous demand, without the need for prior scheduling. Only at the Epsico of UEA16 and at the Student Support Center of Faculdade de Medicina da Universidade Federal de Minas Gerais (Napem/UFMG)27 - the service takes place, respectively, after scheduling by text messages or by filling out an enrollment form, in which the student previously informs the reason for the consultation.
After seeking care, the students usually undergo psychological screening, in which their main complaint or reason for seeking care is verified and the most appropriate intervention is defined. In the Mental Health Care Program (Proasme), implemented by Universidade Federal do Rio de Janeiro (UFRJ), for instance, this initial contact is called “Expanded Reception” and aims to carry out a situational diagnosis based on the assessment of the reasons that led the student to seek the service28.
It was observed that the offered psychological interventions are of different modalities, with a predominance of brief psychoanalytic psychotherapy. This type of intervention is characterized by a reduced number of consultations - from six to ten sessions - with each session lasting about 50 minutes. The main objective of brief psychotherapy is to allow the patient to acquire insight, that is, the knowledge of their psychological reality itself through the interpretation of the reports displayed during the assistance and their living contexts16.
In most studies, it is also emphasized that, in cases of more severe mental disorders or that require long-term approaches, the student is referred to psychological and/or psychiatric care not connected with the educational institution.
Therefore, it would be quite appropriate for the support services to be associated with or establish partnerships with the Psychosocial Care Network (RAPS), which is part of the Brazilian Unified Health System (SUS, Sistema Único de Saúde), in order to guarantee adequate assistance mainly to students recipients of affirmative actions and / or in situations of socioeconomic vulnerability, who cannot afford the costs of a private service.
Other examples of intervention modalities are the psychological-pedagogical or pedagogical guidance provided by the Grapal of FMUSP18),(26 and the prompt psychological assistance (PPA) offered at the Sappe of Unicamp12),(14.
Some support services also have psychiatric care. In this case, the student can request this type of care exclusively or associated with psychological care, as in the Analytical Psychotherapy Service of the Psychiatric Clinic Outpatient Clinic of Hospital das Clínicas de Ribeirão Preto29. Only in the Emotional Reaguard for the Medical Student (Repam), a service of Faculdade de Ciências Médicas da Santa Casa de São Paulo, the prescription of medications by the psychiatrist is reported24. However, there are few services that offer this type of care, probably due to the lack of a psychiatrist working in these projects.
Tutoring or mentoring is another type of offered intervention, as in the Mentoring Program at UFMG20 and in the Mentoring Program of FMUSP19. According to a study published by Leão et al. in 2011, this type of assistance aims to offer a tutor (mentor) to accompany students throughout their training and to promote the exchange of experiences between teachers and students. In this sense, the students are divided into groups, which can vary between 12 to 14 people, with a tutor / teacher being responsible for each group. Regular meetings are held to discuss and guide about aspects related to the medical career and issues relevant to the students’ personal life19.
Many services also work in the development of research and projects that aim to promote mental health within the academic environment and offer subsidies for the improvement of teaching inside the institution. As an example of this performance, we can mention programs that facilitate the student’s integration into the university environment, developed by the Caep of FMRP15),(17, and the scientific production of studies on the student population’s needs. Also in this sense, Caep provides advice to the institution’s Undergraduate Commission, to suggest and implement pedagogical proposals that associate medical training with the well-being of undergraduate students15),(17.
Considering the analyzed data, it is possible to observe that the student support services described in the studies included in this review have the common objective of promoting medical students’ mental health. However, they differ in terms of the offered intervention modalities - ranging from individual assistance to activities in other sectors of the institution -, demonstrating that there is not a single way to effectively address the issue of mental health in Higher Education Institutions. Chart 2 shows the main data collected from the studies included in this review.
Chart 2 Main collected data.
| Author(s)/ Year of Publication | Format/ methodological design | Name of the Service/ Year of Creation | Offered interventions | Target audience | Professionals who constitute the service |
|---|---|---|---|---|---|
| Fernandez and Rodrigues (1993) | Article/ Documental research | Analytical Psychotherapy Service of the Psychiatric Outpatient Clinic of Hospital das Clínicas de Ribeirão Preto, with the year of the service implementation not being informed. Assistance to medical students started in 1983 | Analytical psychotherapy and psychiatric care | Students from courses offered by higher education institutions in São Paulo, among them, Universidade de São Paulo (USP). stands out. The others were not assessed. The greatest demand is from medical and psychology undergraduate students. | Resident physicians of psychiatry, psychology postgraduate students and medical assistants of the institution. |
| Cianflone et al. (2002) | Article/ Historical Description | Educational and Psychological Support Center (CAEP), 1990 | Brief psychotherapy, psychopedagogical guidance, professional guidance, thematic and reflection groups, family guidance, guidance for teachers, guidance and referrals, pedagogical advice to teachers and pedagogical advice to the Graduation Commission. | Undergraduate medical students from Faculdade de Medicina de Ribeirão Preto | Psychologist, educator and academic tech for administrative support |
| Bellodi (2007) | Article/ Observational study | Emotional Rearguard for the Medical Student, of Faculdade de Ciências Médicas da Santa Casa de São Paulo (REPAM), 1997 | Brief psychotherapeutic care with limited time and objectives for students in crisis, referral to care not connected to the institution for individual long-term approaches with limited time, and psychiatric clinical care with the prescription of medications, if necessary. | Students from the Medicine, Speech Therapy and Nursing courses at Faculdade de Medicina da Santa Casa de São Paulo | Psychologists, psychiatrists and secretaries |
| Milian and Arruda (2008) | Article/ Historical Description | Group of Psychological Assistance to Students of Faculdade de Medicina da Universidade de São Paulo (Grapal), created in 1983 and started em 1986 | Psychological and psychiatric assistance to the student, brief preventive psychological interview with students in the first year of the course, organization of events to debate mental health services for students and advice to the family of attended students. | Medical students from FMUSP | Psychologists, psychiatrists, secretary and coordinator |
| Marco (2009) | Article/Essay | Group of Psychological Assistance to Students of Faculdade de Medicina da Universidade de São Paulo (Grapal), the year of creation is not informed. | Open service presentation interview for students in the first year of the course and psychopedagogical support. | Medica students from FMUSP | Not informed in the article |
| Oliveira (2009) | Dissertation/ Documental Research | Psychological and Psychiatric Assistance to Students of Universidade Estadual de Campinas (Sappe/Unicamp), 1987 | Brief psychoanalytic psychotherapy, development of programs that facilitate the student’s integration into the university context, prompt psychological assistance (PPA) and psychiatric clinical care. | Students from the undergraduate and postgraduate courses offered by the higher education institution (Unicamp) | Psychologists and psychiatrists |
| Leão et al. (2011) | Article/ Observational study | Mental Health Service (MHS) and Mentoring Program; the years of creation of services are not informed | Psychological care and monitoring and Mentoring Program | Medical students from a higher education institution (FM-USP) | The mental health service consists of psychologists and psychiatrists and the mentoring program has volunteer teachers who act as mentors. |
| Souza (2011) | Dissertation/ Observational study | The name of the offered service was not informed; its year of creation was 1993 and its year of implantation was 1995 | Psychological and psychiatric care, social work, pedagogical proposals and therapeutic groups with pre-defined subjects | Students from the courses offered by the institution and civil servants (administrative technicians and teachers) | Psychologists, psychiatrists and social workers |
| Campos (2016) | Dissertation/ Documental Research | Psychological and Psychiatric Assistance to Students of Universidade Estadual de Campinas (Sappe/Unicamp), 1987 | Individual consultations for embracement and screening, brief psychotherapeutic interventions with analytical guidance, association with networks and services internal and external to the college, individual, group and relational psychological assistance, prompt psychological assistance (PPA) and emergency psychiatric follow-ups | Medical, nursing and speech therapy students (undergraduate, graduate students and residents), professors and employees from different areas of Unicamp | Psychiatrists and Psychologists |
| Martins and Bellodi (2016) | Article/ Documental Research | The name of the offered service was not disclosed; it was created in 2001 | Mentoring Program | Third-year medical students from Universidade Federal de Minas Gerais (UFMG) | Team of mentors (professions were not informed) |
| Pinho (2016) | Article/ Documental Research | Meio Oeste Catarinense Psychological Assistance Program, 2004 | Psychological care with a cognitive-behavioral approach and students’ referral for treatment with supportive psychotherapy not connected with the institution | In the year of its implantation, it only attended medical students. In 2005, it started to be offered to all students of the other courses offered by the institution | Not informed in the article |
| Malajovich et al. (2017) | Article/ Theoretical-Clinical Reflection | Mental Health Care Program for University students (PROASME); the year the program was created is not disclosed | Open embracement program, with pre-established opening hours, individual interviews aimed at making a situational diagnosis; the therapeutic proposals are diverse and established based on the contact with the student | Students from the courses offered by the higher education institution (not informed in the analyzed article) | Psychologists and psychiatrists who perform interconsultations |
| Murakami et al. (2018) | Article/ Experience Report | Educational and Psychological Support Center (CAEP), 1990 | Psychological screening, brief psychotherapy, educational guidance (psychopedagogical and / or pedagogical), psychological counseling, mentoring program in the Mentoring category, psychopedagogical and pedagogical guidance workshops, reflection groups and focal groups, consultancy services to the Graduation Commission and teachers of the institution | At the time of its creation, it attended only medical students, being subsequently expanded to courses in physical therapy, speech therapy, nutrition, occupational therapy, biomedical informatics and biomedical science. | Three psychologists, a psychopedagogue, a pedagogue and an administrative technician |
| Neves et al. (2019) | Article/ Experience Report | Psychosocial Care Space (EPSICO), having been conceived and proposed in 2015 and implemented in 2018 | Brief psychotherapeutic psychological assistance based on individual consultations; offer of professional internship in the field of psychology as of 2019 | Students of the courses offered by the higher education institution | At the time of its creation, it had five psychologists and an occupational therapist. It currently consists of three psychologists |
| Mendes (2019) | Article/ Historical Description | Psychological Assistance to PUC Minas Students (APP),created in 2002 | The students’ psychosocial embracement was carried out through listening, brief psychotherapeutic care in cases of subjective urgency and referral to psychological care not connected with the institution for longitudinal follow-ups | Students from the Institution | Psychologists, monitors and psychology interns. |
| Ribeiro et al. (2019) | Article/ Documental Research | Student Psychopedagogical Support Center of FM-UFMG (NAPEM), 2004 | Psychological interventions after the filling out of an enrollment form by the student | FM-UFMG students enrolled in medicine, speech therapy and radiology technology courses | Not informed in the article |
Target audience
All the mental health support services described in the selected studies attend medical students. However, some of these services are also available to undergraduate students from other courses.
Overall, one can observe that most support services were implemented aiming at providing psychological and psychopedagogical assistance only to medical students, possibly due to the higher prevalence of mental disorders in this group, as shown by Pacheco et al. (2017). As an example, we have the Universidade do Oeste de Santa Catarina Student Support Service (Unoesc), implemented in 2004 to assist medical students21.
With the expansion of the service and/or the implementation of other courses in the institutions, some mental health care services also started to attend students from other undergraduate courses, such as the Caep of FMRP, which, in 2002, started to meet the demands of other courses in the health area, such as Physical Therapy, Speech Therapy and Nutrition15. In only one of the included studies, the assessed service also attended students regularly enrolled in the institution’s postgraduate program12.
Professionals involved
Mental health support services consist, in most cases, of multiprofessional teams that vary in number and in the involved professional categories.
Services that offer psychological and psychiatric care commonly consist of psychologists and psychiatrists. Teams may also include psychopedagogues, pedagogues, administrative technicians, secretaries and occupational therapists. The APP of PUC Minas23 and the Analytical Psychotherapy Service of the Psychiatric Outpatient Clinic of Hospital das Clínicas de Ribeirão Preto29 also have interns from the Psychology undergraduate course and resident physicians in Psychiatry, respectively.
The tutoring or mentoring programs offered by the medical schools of USP19 and UFMG20, on the other hand, consist of teachers from the undergraduate course, usually on a voluntary basis.
In three of the included studies, there is no information about the professionals who constitute the assistance service21),(26),(27.
It is noteworthy that some services show some instability regarding the number of professionals. In the study that describes the Epsico of UEA, it is reported that, in 2015, the year the project was created, the service had five psychologists and an occupational therapist. However, in the year the article was prepared, in 2019, only three psychologists worked in the service16.
It can be assumed that the lack of a fixed professional staff is a factor that hinders the development of long-term projects, as well as the consolidation and expansion of mental health support services in Brazilian higher education institutions.
FINAL CONSIDERATIONS
The strengths of this review were the systematic and comprehensive search in the literature, as well as the knowledge gaps found based on the information collected from the included studies.
Considering the obtained results, it was observed that mental health support services addressed by the studies have the common objective of promoting mental health and, therefore, the medical student’s quality of life. Different types of intervention, through individual and / or collective meetings, aim to welcome and support the students in their academic, psychological and social demands.
Most support services provide a first embracement to the student, set up as a listening space, and short-term interventions, with a predominance of brief psychotherapy. The access to these services depends, in general, on the university students’ own initiative to seek them out, in the presence of any complication that might result in damage to their mental health.
However, some limitations were found when carrying out the study. Publications on student support services are scarce when compared to the number of institutions that offer an undergraduate medical course in Brazil. Moreover, the studies have a more descriptive character, when the ideal would be to have, in addition to the description, an assessment of the interventions offered by the support services, which would be more relevant than the experience reports.
Most of the available publications were carried out by public higher education institutions in the Southeast region, which makes it difficult to map and identify information about support services offered by institutions in other regions of the country.
The predominance of studies that report support services in public higher education institutions may suggest a publication bias. It is possible that other private teaching institutions have services for their students; however, for reasons not identified in this research, do not publish on the topic.
It is also important to highlight that the studies do not disclose the socioeconomic profile of the students assisted by the support services, nor is there mention of the presence of students who entered the university through the quota system or who are supported by the permanence policies. Knowledge about this profile would be important for the development of assistance strategies for students, especially to guarantee that the economically vulnerable group receive the adequate treatment follow-up.
Another limitation is the fact that most of the studies included in this review do not detail how to implement the services or how the proposed interventions are put into practice. Additionally, there was no information on possible difficulties in maintaining a multiprofessional team or on the impact of interventions on the attended students’ mental health.
In addition, it is worth recognizing that many other actions aimed at promoting mental health are carried out in the academic environment by mental health fronts, leagues and other sectors unrelated to support services, and, therefore, were not part of this review.
As for the relationship between educational institutions and support services, it was observed that, despite their decisive role in the process of creating these services, there is no information in the studies regarding the participation of academic management at other times. It was not addressed, for instance, whether the teaching centers develop regular actions to promote mental health in the academic context, or whether there is a concern to carry out curricular and organizational changes aiming to meet the mental health demands.
Finally, although the main objective of this review was to map, through publications, the mental health support services that exist in higher education institutions in Brazil, one cannot infer that the services described in the included studies are still active. It is also possible that changes have occurred, both in the operation and composition of services.
These gaps indicate the need for more research on medical students’ mental health care, as well as greater institutional incentive for the development of projects and studies with this focus. It is expected that, through further research on this topic, discussions on mental health can be expanded and strategies that prove to be effective can be implemented in students’ support services, aiming to expand and consolidate the actions of these services in higher education institutions in Brazil.











 texto em
texto em