Serviços Personalizados
Journal
Artigo
Compartilhar
Revista Brasileira de Educação Médica
versão impressa ISSN 0100-5502versão On-line ISSN 1981-5271
Rev. Bras. Educ. Med. vol.46 no.3 Rio de Janeiro 2022 Epub 18-Ago-2022
https://doi.org/10.1590/1981-5271v46.3-20210314
ORIGINAL ARTICLE
Medical identity: the impact of first contact with patient in medicine student’s empathy
1Universidade Federal de Minas Gerais, Belo Horizonte, Minas Gerais, Brazil.
Introduction:
Empathy is defined as the ability to listen and understand the other, thus becoming an essential component in the doctor-patient relationship. Studies indicate that the opportunity to make contact with the patient early in the course raises awareness of the importance of empathy in the relationships. Thus, such contact, in the first semesters of medical school, enables students to enhance their empathic skills, permitting the construction of a broader and more complete professional identity.
Objective:
The study aims to evaluate the influence on the empathy of medical students through the interaction with patients in the discipline of Semiology I, during the second year of undergraduate school.
Method:
Observational and prospective study with medical students from a private medical school in Vitória (ES), enrolled in the theoretical-practical discipline of Semiology I in 2019/2 and 2020/1, through the application of questionnaires, before the first practical activity in the ward and after the last one. Sociodemographic variables and empathy score were analyzed. The differences between the semesters were evaluated by Chi-square, Fisher’s exact or Mann-Whitney tests. The relationship between sociodemographic variables and empathy was assessed by the Mann-Whitney and Kruskal-Wallis tests. The influence of contact with patients on students’ empathy was analyzed by the Wilcoxon test, all with 95% significance.
Results:
The sample consisted of 38 students in 2019/2 and 60 in 2020/1. Only the associations between contact with the patients in the wards and the empathy score (p=0.008) and gender and the empathy score (p=0.000) were significant; empathy was greater among women and at the end of the discipline experience.
Conclusion:
The interaction between medical students and patients during the discipline of Semiology I was able to positively affect empathy, corroborating the literature. The higher levels of empathy among women also corroborate the literature. The obtained results reflect only a specific semester of the course, not the students’ overall empathy profile, levels of empathy at different moments of undergraduate school, or their behavior.
Keywords: Empathy; Medical Education; Physician-Patient Relationship; Patient-Centered Care
Introdução:
Empatia é definida como a capacidade de ouvir e compreender o outro, e, portanto, é um componente essencial na relação médico-paciente. Estudos apontam que proporcionar aos alunos a oportunidade de contato com o paciente logo no início do curso desperta a consciência da importância da empatia nas relações. Dessa forma, tal contato, nos primeiros semestres da Faculdade de Medicina, permite que os estudantes potencializem suas habilidades empáticas, oportunizando a construção de uma identidade profissional mais ampla e completa.
Objetivo:
O estudo tem como objetivo avaliar a influência do contato com o paciente na disciplina de Semiologia I, durante o segundo ano da graduação, sobre a empatia de estudantes de Medicina.
Método:
Trata-se de um estudo observacional e prospectivo, realizado com estudantes de Medicina de uma faculdade privada em Vitória, no Espírito Santo, matriculados na disciplina teórico-prática Semiologia I em 2019/2 e 2020/1, por meio de aplicação de questionários antes da primeira atividade prática em enfermaria e após a última. Analisaram-se as variáveis sociodemográficas e o escore de empatia. Diferenças entre os semestres foram avaliadas pelos testes qui-quadrado, exato de Fisher e de Mann-Whitney. Com os testes de Mann-Whitney e Kruskal-Wallis, investigou-se a relação entre as variáveis sociodemográficas e a empatia. A influência do contato com o paciente na empatia foi averiguada pelo teste de Wilcoxon, todos com 95% de significância.
Resultado:
Participaram do estudo 38 alunos em 2019/2 e 60 em 2020/1. Foram significativas somente as associações entre o contato com o paciente nas enfermarias e o escore de empatia (p = 0,008), e entre o sexo e o escore de empatia (p = 0,000), sendo esta maior para mulheres e ao final da experiência da disciplina.
Conclusão:
A disciplina Semiologia I se mostrou capaz de afetar positivamente a empatia, que se apresentou maior no sexo feminino, corroborando a literatura. Os resultados obtidos refletem somente um semestre específico do curso, não o perfil global de empatia dos estudantes, os níveis de empatia em momentos distintos da graduação ou o comportamento dos discentes.
Palavras-chave: Empatia; Educação Médica; Relações Médico-Paciente; Assistência Centrada no Paciente
INTRODUCTION
Empathy derives from the Greek word empatheia (em = inside and pathos = suffering or feeling) and is defined as a genuine disposition to be able to hear and understand the other1, thus becoming an essential component of interpersonal communication. Studies have proposed that empathy includes cognitive and emotional attributes, which makes it multidimensional in a context permeated by cultural, affective, behavioral and moral aspects2.
In medical practice, the development of empathy is related to clinical competence and the reduction in medical errors3. Once introduced as a component of the doctor-patient interaction4, empathy proved to be beneficial for increasing patient adherence to treatment, reducing medical malpractice complaints and increasing favorable outcomes related to the illness process. Additionally, it was observed that the empathic relationship between doctor and patient has a positive impact on health professionals’ health, well-being and satisfaction, by promoting more constructive, consistent and integral experiences between the parties. However, the current scenario in medical schools suggests that, throughout undergraduate school, medical students report a decline in their own empathy, a fact that is a matter of concern for the future of medical practice5.
In the mid-twentieth century, opportunities were provided, at a global level, for the development of a scientistic vision, resulting in a new model for the concept of health and illness. This effect significantly contributed to moving medical practice away from clinical care, making it difficult for physicians to see illness as a set of factors6. The Schools of Medicine may have contributed to medical dehumanization, given that the application of attitudes and behaviors linked to humanization was attributed only to personal experiences and family education experienced by the student, without any approach during the course7.
From this perspective, there is currently an overall concern about the decrease in empathy levels among medical students. Countries such as Iran, New Zealand and the United States of America have shown that the decline in empathy is a common problem in their respective undergraduate medical courses4. The critical view of the empathy levels in medical courses also showed that, in western countries, empathy scores were higher when compared to eastern empathy scores. One of the reasons for the global decline and the difference in empathy scores between different countries is the low integration of communication and humanistic skills in medical curricula8. Aiming to change the current situation, councils and associations, such as the General Medical Council of the United Kingdom and the Association of American Medical Colleges, started to incorporate the development of empathy into guidelines and recommendations for medical courses and medical practice9.
In Brazil, the concern and the adoption of coping measures in the presence of the decrease in empathy among medical students are no different. Therefore, since 2001, with the creation of the National Curriculum Guidelines for the Undergraduate Course in Medicine and its update in 2014, there has been an attempt to prioritize a generalist, humanist, critical and reflective medical training, demanding from the student skills that enable a greater understanding and a broader scope of the doctor-patient relationship, such as empathy6. However, the initiative faces challenges that are closely related to the formation of the medical professional identity and, consequently, to the students’ empathy: the logistics of academic curriculum planning, the relationship of students with teachers and patients during undergraduate school and the personal sociodemographic factors of each undergraduate student3.
To measure empathy in medical students, the Jefferson Empathy Scale for Medical Students (JSE) has been used. This psychometric measurement instrument is a validated tool, consisting of 20 questions, which analyze three main factors of cognitive empathy: “perspective-taking”, “compassionate care” and “standing in patients’ shoes” (9. Widely disseminated in scientific research, this tool has become a great help in the assessment of empathy in the doctor-patient interaction. However, it is known that, as it only assesses the cognitive aspect of empathy, research that goes beyond the JSE is necessary to encompass the several areas involved in the construction of empathy10.
In this context, the medical students’ early and frequent exposure to the knowledge and skills related to essential competencies for a health professional are essential for a better understanding and a better performance regarding the interaction with patients10. Thus, providing contact with the patient at the beginning of the course raises awareness of the importance of empathy in relationships, giving future doctors the possibility to further develop their empathic skills, constructing a broader and more thorough professional identity1.
The aim of this study is to evaluate the influence of the contact with patients on medical students’ empathy, in a private medical school located in Vitória (ES), attending the third semester of undergraduate medical school.
METHODS
This was an observational, prospective study, carried out through by applying a questionnaire to medical students from a private school in Vitória, state of Espírito Santo (ES), Brazil, regularly enrolled in the Semiology I discipline in the academic semesters of 2019/2 and 2020/1.
The course takes place twice-yearly and includes theoretical and theoretical-practical classes, in which students learn to perform physical exams and build anamnesis. The practical classes involve the participation of patients admitted to the teaching hospital wards. Within the course curriculum, Semiology I provides the first effective contact between students and patients.
The target population comprised 60 students in the 2019/2 semester and 88 students in the 2020/1 semester, totaling 148 students. Those who agreed to participate in the study were included and those who had errors or omissions when filling out the research forms were excluded. At the end of the selection process, 98 students constituted the study population.
A questionnaire with sociodemographic variables (age, gender, average monthly family income, marital status, religion, student’s level of schooling, father’s level of schooling, mother’s level of schooling, paid work, participation in extracurricular activities, living with parents, close family member working in the health area, incentive to study medicine, significant previous experience with illness in the family, desired specialty) and the student version of the JSE were applied at the beginning of each academic semester.
This scale assesses the level of empathy in medical students and consists of three axes of analysis: compassionate care, the ability to stand in the patient’s shoes, and perspective-taking. The axes are divided into 20 questions, which are answered using a Likert scale. This scale consists of 7 items, graded from 1 to 7. There are affirmative questions, where 1 means “strongly disagree” and 7 means “strongly agree”; and there are negative questions, in which this logic is the opposite. Alternatives 2, 3, 5 and 6 correspond to increasing levels of agreement, in the case of affirmative questions, and decreasing levels of agreement, in the case of negative questions. Number 4 denotes indifference to what is asked. The three mentioned axes, in sequence, can have minimum and maximum scores between 11 and 77, between 2 and 14 and between 7 and 49. This totals an overall score between 20 and 140 points. The scale does not include a cutoff point, and a higher score is related to greater empathy.
At the end of the 2019/2 academic semester, the JSE was applied again. However, due to the Sars CoV-2 pandemic, the application of the scale at the end of the 2020/1 academic semester was compromised by the suspension of all theoretical-practical classes at the institution.
A description of the second semester sample was carried out through the distribution of frequencies for qualitative variables and the mean and standard deviation for age and score at the start of the semester. The differences between the academic semesters were evaluated at a 95% significance level using Pearson’s Chi-square or Fisher’s Exact test for qualitative variables and the Mann-Whitney U-test for independent samples for quantitative variables.
The normality of the variables age and empathy score was evaluated by the Kolmogorov-Smirnov test, with a 95% significance.
To define the students’ empathy profile, the mean and standard deviation of the empathy scores observed in all students included in the survey and who completed the questionnaire at the start of the two academic semesters were categorized according to sociodemographic data. An association analysis was performed using the Mann-Whitney test for independent samples for dichotomous qualitative variables. The Kruskal-Wallis test was used for ordinal qualitative variables, with a 95% significance.
The influence of the contact with patients on student empathy was assessed only with students who participated at the start and the end of the 2019/2 academic semester, evaluated by the Wilcoxon Signed Rank test for paired samples, with a 95% significance.
This research project was approved by CEP under CAAE number 09706919.7.0000.5065.
RESULTS
In the 2019/2 academic semester, 60 questionnaires were applied at the start and the end of the semester; 15 students did not fill out one of the questionnaires, one student did not answer the JSE questions and 6 students did not fill out any of the questionnaires, totaling 38 students who were included in the study. In the academic semester of 2020/1, 88 questionnaires were applied, of which 60 were correctly filled out. In total, 98 students were included in the study.
Students from the 2019/2 and 2020/1 academic semesters were similar regarding the sociodemographic characteristics and the initial score in the JSE (Table 1). Considering the set of semesters, an initial score was observed with a minimum and maximum value of 83 and 138, respectively, mean and standard deviation of 119.84 and 10.73, respectively. The median, first and third quartiles were 122, 114, and 127, respectively.
Table 1 Sample characteristics according to the academic semester.
| Variables | 2019/2 | 2020/1 | Total | p-value | ||||
|---|---|---|---|---|---|---|---|---|
| No | % | No | % | No | % | |||
| Gender | Female | 26 | 68.42 | 35 | 58.33 | 61 | 62.24 | 0.316a |
| Male | 12 | 31.58 | 25 | 41.67 | 37 | 37.76 | ||
| Age b | 20.00 | 2.19 | 20.03 | 2.75 | 20.02 | 2.54 | 0.898c | |
| Marital status | In a relationship | 11 | 28.95 | 15 | 25.00 | 26 | 26.53 | 0.666a |
| Single | 27 | 71.05 | 45 | 75.00 | 72 | 73.47 | ||
| Mean family income | 1 |-- 5,000 | 8 | 21.05 | 5 | 10.00 | 13 | 14.28 | 0.333a |
| 5 |-- 10,000 | 6 | 15.79 | 7 | 11.67 | 13 | 13.27 | ||
| 10 |-- 20,000 | 9 | 23.68 | 13 | 21.67 | 22 | 22.45 | ||
| 20 |-- 50,000 | 11 | 28.95 | 21 | 35.00 | 32 | 32.65 | ||
| |-- 50,000 | 4 | 10.53 | 13 | 21.67 | 17 | 17.35 | ||
| Religion | No | 7 | 18.42 | 16 | 26.67 | 23 | 23.47 | 0.348a |
| Yes | 31 | 81.58 | 44 | 73.33 | 75 | 76.53 | ||
| Previous Higher Education degree | No | 35 | 92.11 | 51 | 85.00 | 86 | 87.76 | 0.359d |
| Yes | 3 | 7.89 | 9 | 15.00 | 12 | 12.24 | ||
| Paid work | No | 38 | 100.00 | 60 | 100.00 | 98 | 100.00 | - |
| Yes | 0 | 0.00 | 0 | 0.00 | 0 | 0.00 | ||
| Extracurricular Activities in Medical School | No | 20 | 52.63 | 40 | 66.67 | 60 | 61.22 | 0.165a |
| Yes | 18 | 47.37 | 20 | 33.33 | 38 | 38.78 | ||
| Paternal Higher Education degree | No | 10 | 26.32 | 13 | 21.67 | 23 | 23.47 | 0.597a |
| Yes | 28 | 73.68 | 47 | 78.33 | 75 | 76.53 | ||
| Maternal Higher Education degree | No | 7 | 18.42 | 10 | 16.67 | 17 | 17.35 | 0.823a |
| Yes | 31 | 81.58 | 50 | 83.33 | 81 | 82.65 | ||
| Lives with parents | No | 7 | 18.42 | 19 | 31.67 | 26 | 26.53 | 0.148a |
| Yes | 31 | 81.58 | 41 | 68.33 | 72 | 73.47 | ||
| Family member working in the health area | No | 17 | 44.74 | 17 | 28.33 | 34 | 34.69 | 0.096a |
| Yes | 21 | 55.26 | 43 | 71.67 | 64 | 65.31 | ||
| Incentive for Medicine | No | 12 | 31.58 | 16 | 26.67 | 28 | 28.57 | 0.600a |
| Yes | 26 | 68.42 | 44 | 73.33 | 70 | 71.43 | ||
| Experience of illness | No | 10 | 26.32 | 19 | 31.67 | 29 | 29.59 | 0.572a |
| Yes | 28 | 73.68 | 41 | 68.33 | 69 | 70.41 | ||
| Specialty | No | 23 | 60.53 | 29 | 48.33 | 52 | 53.06 | 0.239a |
| Yes | 15 | 39.47 | 31 | 51.67 | 46 | 46.94 | ||
| Initial score b | 121.68 (8.61) | 118.67 (11.80) | 119.84 (10.73) | 0.300c | ||||
Notes: a Pearson’s chi-square test
b Mean (standard deviation)
c Mann-Whitney U-test for independent samples
d Fisher’s Exact Test
According to Table 1, the sample predominantly consisted of female students aged 20 years ± 2.54, students who declared having a religion, being single, not having another higher education degree and not participating in extracurricular activities. Most of these students live with their parents, with at least one of the latter having complete or incomplete higher education, with a family income greater than R$10,000 and less than R$40,000; they also have family members working in the health area, were encouraged by someone to study medicine, had some significant personal or family experience with illness and have not yet decided which medical specialty they will pursue after completing the course.
Table 2 shows the results of the initial score in the JSE according to the assessed variables. There was a statistically significant difference in the scores between the genders (p=0.000), with men showing a mean and standard deviation of 115.2 and 11.2, respectively. For women, they were 122.6 and 9.5, respectively.
Table 2 Scores in the Jefferson Scale of Empathy at the beginning of the 2019/2 and 2020/1 academic semesters, according to sociodemographic variables.
| Variables | Mean | Standard deviation | p-value | |
|---|---|---|---|---|
| Gender | Female | 122.6 | 9.5 | 0.000a |
| Male | 115.3 | 11.2 | ||
| Marital status | In a relationship | 119.3 | 11.5 | 0.888a |
| Single | 120.0 | 10.5 | ||
| Mean family income | 0 |-- 5,000 | 123.8 | 10.3 | 0.249b |
| 5 |-- 10,000 | 121.2 | 11.0 | ||
| 10 |-- 20,000 | 116.0 | 13.3 | ||
| 20 |-- 50,000 | 119.8 | 9.2 | ||
| |-- 50,000 | 120.5 | 9.4 | ||
| Religion | No | 118.4 | 9.3 | 0.222a |
| Yes | 120.3 | 11.2 | ||
| Previous Higher Education degree | No | 120.0 | 10.8 | 0.519a |
| Yes | 118.4 | 10.3 | ||
| Paid work | No | - | - | - |
| Yes | 119.8 | 10.7 | ||
| Extracurricular activity in medical school | No | 120.3 | 10.4 | 0.545a |
| Yes | 119.1 | 11.3 | ||
| Paternal Higher Education degree | No | 121.0 | 12.2 | 0.298a |
| Yes | 119.5 | 10.3 | ||
| Maternal Higher Education degree | No | 123.4 | 9.8 | 0.116a |
| Yes | 119.1 | 10.8 | ||
| Lives with parents | No | 118.7 | 13.4 | 0.949a |
| Yes | 120.2 | 9.7 | ||
| Family member working in the health area | No | 120.5 | 11.5 | 0.528a |
| Yes | 119.5 | 10.4 | ||
| Incentive for Medicine | No | 118.6 | 9.8 | 0.306a |
| Yes | 120.3 | 11.1 | ||
| Experience of illness | No | 117.3 | 11.7 | 0.128a |
| Yes | 120.9 | 10.2 | ||
| Specialty | No | 120.9 | 10.3 | 0.293a |
| Yes | 118.7 | 11.2 | ||
Notes: There was no correlation between age and the initial score (Spearman’s correlation: p value=0.066).
a = by the Mann-Whitney test.
b = by the Kruskal-Wallis test.
Despite the statistical significance, and observing the sociodemographic variables in Table 2, students who reported having a religion, living with their parents, having been encouraged by someone to study medicine and having had a relevant experience with illness in the family had a higher mean score, as well as single students. The students’ involvement in extracurricular activities, the definition of a specialty at the end of the course and the level of schooling of the student and both parents, considered here as having complete or incomplete higher education, was not related to higher average empathy scores.
It was not possible to observe an evident relationship between the average levels achieved in the JSE in relation to the average family income, with the lowest average score being observed for the income range between R$ 10,000 and R$ 19,999 and the highest score for the income range lower than BRL 5,000. The association between age and the empathy score was also not statistically significant (p=0.066). In relation to age, as shown in Figure 1, it was also not possible to observe an obvious relationship between the means of the empathy score and the different ages.
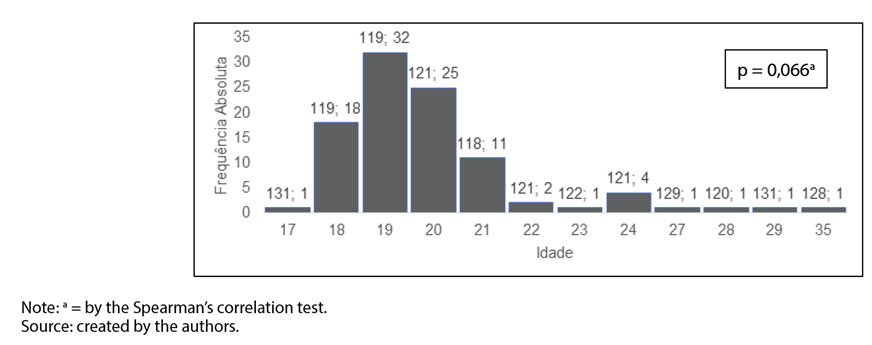
Figure 1 Histogram showing the students’ age distribution for the academic semesters of 2019/2 and 2020/1. At the top of the bars, respectively, are the average empathy scores and absolute frequencies for each age.
An association was also observed between contact with the patient in the wards and the empathy score (p=0.008), when the evolution of this variable was studied between the start and the end of the 2019/2 school semester. The descriptive results of the initial and final applications of the JSE in the abovementioned semester are shown in Table 3.
Table 3 Score statistics in the Jefferson Empathy Scale at the beginning and the end of the 2019/2 school semester.
| Statistics | Initial score | Final score |
|---|---|---|
| Minimum | 104.00 | 82.00 |
| Maximum | 135.00 | 138.00 |
| Mean | 121.68 | 123.66 |
| Standard deviation | 8.61 | 11.52 |
| Median | 122.50 | 128.00 |
| 25 th percentile | 115.00 | 119.00 |
| 75 th percentile | 129.00 | 131.00 |
Note: The median of the differences between the scores showed a statistically significant difference (Wilcoxon signed rank tests for related samples: p value=0.008).
DISCUSSION
After analyzing the results, it was observed that stimulating contact with the patient in the Semiology I module was significantly effective in increasing the empathy score of the students attending the 2019/2 academic semester. Although previous studies did not explore the students’ first contact with patients in a hospital context, the results of this research corroborate studies on the subject, indicating that practical experience and the exercise of communication are crucial factors for the development of empathy. These factors provide learning experiences without the demands and pressure inherent to the profession and, at the same time, allow students to improve their patient management skills and to reflect on the lived experiences11. Therefore, the continuous and early exposure of medical students to environments of practical activities solidifies not only the academic experience but also the students’ understanding of their own behaviors and the impact of actions on the doctor-patient relationship10.
However, it is known that the development of empathy comprises a complex dialogue5 between individual, environmental and academic aspects11, and cannot be summarized only in the context of practical activities carried out during undergraduate school. Research suggests that the level of empathy in medical students is closely related to the cultural aspect and sociodemographic characteristics that permeate the entire student’s experience12.
From this perspective, regarding the cultural aspect, studies that compared the levels of empathy between countries13 and even between the Western and Eastern hemispheres8 are highlighted, revealing, based on the difference in results in each region, that cultural influence has an impact on the construction of the empathy conception in individuals.
In relation to the sociodemographic characteristics, our study aimed to analyze them, showing that only the variable gender was an influencing factor regarding the empathy score. Concerning this variable, the results confirm the scientific information, disseminated worldwide, that women have significantly higher levels of empathy, according to the JSE, when compared to men14. It is believed that the high levels of empathy among women are due to greater sensitivity to emotional states, as shown by research3.
Particularly, the initial hypothesis of this study about sociodemographic variables indicated, in addition to gender, religion, previous experience of personal and/or family member illness, age and specialization as potential variables that influence the development of empathy in medical students. However, the last four did not prove to be statistically significant.
Our finding differs from those of other studies, which concluded that the variables religion (having a religion), age (students older than the mean age) and choice of specialization (students who consider internal medicine rather than surgery) also have a significant positive influence on empathy12. This difference can be due to the cultural aspects, widely explored as influencing empathy, as well as by the difference between the research samples, either by the number of participants, or by the context in which they were included in the undergraduate course, such as the difference between semesters.
The variable previous experience of illness, in turn, was not explored in previous studies, therefore not allowing the comparison. However, we believe that it should be explored in further studies, considering its possible relevance in the construction of subjective empathy, an aspect of empathy that is not explored in the JSE (it explores only the so-called cognitive empathy).
Throughout our study, empathy proved to be a topic of extreme relevance and comprehensiveness worldwide. Thus, even though many studies are being carried out, several fields have yet to be explored. One of the challenges is to correlate a complex virtue that is related both to the cognitive scope, which can be quantified by the JSE14, as well as to the subjective scope, which may, therefore, vary according to different points and contexts to be evaluated9. In the subjective context, research has revealed, for instance, that the pressure, lack of support and exhaustion generated by medical school play an important role in the reduction of empathy among students5, a fact that justifies the scientific results of its decline throughout the medical course.
The National Curriculum Guidelines guide the undergraduate courses and, in the medical course, they also advocate empathy as an inherent characteristic of the medical professional15. Therefore, they lead the educational institutions to consider its approach during undergraduate school. In this study, it was possible to verify that this competence is academically treated in an indirect way, regarding the addressed subject, permeating the students’ behavior during the performance of the physical examination and the preparation of the anamnesis through the interview with the patient.
Hence, it is necessary to show empathy in the discipline schedules, observing the prerogative of the curricular guidelines, enhancing the skills of professionals in training.
Studies that aim to innovate the understanding of empathy and to promote academic changes that elevate humanistic knowledge to an actual relevance in the formation of a student’s medical identity2, are and will be important support tools, both for students and for educational institutions, in an attempt to implement and enhance empathic skills in the medical environment and, consequently, to optimize medical practice.
During the application of the sociodemographic and JSE questionnaires, some deficiency was observed regarding their completion by the students, which culminated in the exclusion of participants in the 2019/2 semester. Additionally, during the 2020/1 school semester, the COVID-19 pandemic started all over the world. At the beginning of the academic semester, there were still in-person classes in Brazil, since the virus was not in circulation yet; however, on 03/16, the institution participating in the research, together with the Ministry of Education, decided to postpone in-person classes until more information could be obtained. With the advancement of the pandemic, the distance learning model was implemented. This fact prevented the assessment of the effect of contact with patients on the students’ empathy in the class attending that semester, since visits to the wards were suspended. Moreover, the obtained empathy scores reflect only one semester (3rd semester) of the undergraduate medical school at a private school in Brazil and not the global profile of medical students, regardless of the attended semester.
CONCLUSION
The obtained results corroborate the literature in relation to greater empathy among women and in the sense that a practical experience, in this case the discipline of Semiology I, is able to positively affect the empathy of medical students, resulting in a professional profile increasingly in line with the National Curriculum Guidelines for the Undergraduate Course in Medicine. Empathy is still not objectively addressed in this discipline and doing so can improve the learning of this competence.
We expect that new studies will be able to cover comparisons of scores between different classes or that they can follow the course of a given class, in different institutions, aiming to understand the actual effect of contact with patients on the development of students’ empathy, throughout the medical course and in the different pedagogical contexts, as well as what possible variables would positively or negatively influence the level of empathy.
REFERENCES
1. Thomazi L, Moreira FG, Marco MA. Avaliação da empatia em alunos do 4º ano da graduação em Medicina da Unifesp em 2012. Rev Bras Educ Med. 2014;38(1):87-93. [ Links ]
2. Eikeland H, Ørnes K, Finset A, Pedersen R. The physician’s role and empathy: a qualitative study of third year medical students. BMC Med Educ. 2014 Aug;14(165):[about 8 p.]. doi: https://doi.org/10.1186/1472-6920-14-165. [ Links ]
3. Park KH, Kim D, Kim SK, Yi YH, Jeong JH, Chae J, et al. The relationships between empathy, stress and social support among medical students. Int J Med Educ. 2015 Sept;6:103-8. [ Links ]
4. Mahoney S, Sladek RM, Neild T. A longitudinal study of empathy in preclinical and clinical medical students and clinical supervisors. BMC Med Educ . 2016 Oct;16(270):[about 8 p.]. doi: https://doi.org/10.1186/s12909-016-0777-z. [ Links ]
5. Smith KE, Norman GJ, Decety J. The complexity of empathy during medical school training: evidence for positive changes. Med Educ. 2017 Nov;51(11):1146-59. [ Links ]
6. Nascimento HCF, Ferreira Júnior WA, Silva AMTC, Carvalho IGM, Bastos GCFC, Anchieta RJ. Análise dos níveis de empatia de estudantes de Medicina. Rev Bras Educ Med . 2018;42(1):150-8. [ Links ]
7. Dell Amore Filho E, Dias RB, Toledo Jr ACC. Ações para a retomada do ensino da humanização nas escolas de Medicina. Rev Bras Educ Med . 2018;42(4):14-28. [ Links ]
8. Tariq N, Rasheed T, Tavakol M. A quantitative study of empathy in Pakistani Medical students: a multicentered approach. J Prim Care Community Health. 2017 Oct;8(4):294-9. [ Links ]
9. O’Tuathaigh CMP, Idris AN, Duggan E, Costa P, Costa MJ. Medical students’ empathy and attitudes towards professionalism: Relationship with personality, specialty preference and medical programme. PLoS One. 2019;14(5):[about 15 p.]. doi: https://doi.org/10.1371/journal.pone.0215675. [ Links ]
10. Zanetti ML, Dinh A, Hunter L, Godkin MA, Ferguson W. A longitudinal study of multicultural curriculum in medical education. Int J Med Educ . 2014 Feb;5:37-44. [ Links ]
11. Pohontsch NJ, Stark A, Ehrhardt M, Kötter T, Scherer M. Influences on students’ empathy in medical education: an exploratory interview study with medical students in their third and last year. BMC Med Educ . 2018 Oct;18(231):[about 9 p.]. doi: https://doi.org/10.1186/s12909-018-1335-7. [ Links ]
12. Dehning S, Gasperi S, Tesfaye M, Girma E, Meyer S, Krahl W, et al. Empathy without borders? Cross-cultural heart and mind-reading in first-year medical students. Ethiop J Health Sci. 2013 July;23(2):113-22. [ Links ]
13. Wen D, Ma X, Li H, Liu Z, Xian B, Liu Y. Empathy in Chinese medical students: psychometric characteristics and differences by gender and year of medical education. BMC Med Educ . 2013 Sept;13(130):[about 6 p.]. doi: https://doi.org/10.1186/1472-6920-13-130. [ Links ]
14. Valente AF, Costa P, Elorduy M, Virumbrales M, Costa MJ, Palés J. Psychometric properties of the Spanish version of the Jefferson Scale of Empathy: making sense of the total score through a second order confirmatory factor analysis. BMC Med Educ . 2016 Sept;16(242):[about 12 p.]. doi: https://doi.org/10.1186/s12909-016-0763-5. [ Links ]
15. Brasil. Resolução nº 3, de 20 de junho de 2014. Institui Diretrizes Curriculares Nacionais do Curso de Graduação em Medicina e dá outras providências. Diário Oficial da União, Brasília; 23 jun 2014. Seção 1, p. 8-11. [ Links ]
Received: September 02, 2021; Accepted: May 28, 2022











 texto em
texto em 



